Mode switch during atrial arrhythmias
Content
General information
The management of pacemaker patients with atrial arrhythmia episodes is complex, due to the different types of mechanisms known to trigger atrial arrhythmias, and the risk of ventricular pacing running out of control on detection of a rapid atrial rhythm.
Detection of atrial arrhythmias is an ongoing process in which the device analyzes the atrial rate and its effect on the ventricular rhythm. The stimulator automatically records diagnostic data on the various arrhythmia episodes, which can help in the management of these patients and in any therapeutic adaptation.
The device can be programmed to respond to an atrial arrhythmia by switching to an asynchronous mode, to avoid high-frequency ventricular pacing that could compromise hemodynamic stability. Mode switching refers to the pacemaker’s ability to switch automatically from an atrial tracking mode (DDD or VDD) to a non-atrial tracking mode (DDI or VDI). The ventricular pacing frequency gradually shifts (depending on the manufacturer) from synchronous to tracking frequency. This avoids a sudden drop in ventricular rate. When the atrial tachyarrhythmia ends, mode switching returns to the programmed synchronous pacing mode.
The ideal mode switching algorithm has the following features:
- rapid triggering to avoid prolonged rapid ventricular pacing during the initial arrhythmia detection phase
- ability to quickly switch back to synchronous mode at the end of the arrhythmia episode
- good ability to diagnose atrial arrhythmia even in the presence of atrial signals of variable amplitude and frequency
- ability to avoid mode switching in response to cross-talk, noise or sinus tachycardia
Brand specific information
Abbott
Mode switching algorithm
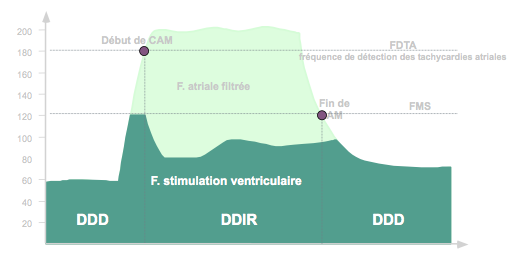
Automatic mode switching (AMS) takes place when the filtered atrial frequency exceeds the atrial tachycardia detection frequency (ATDF).
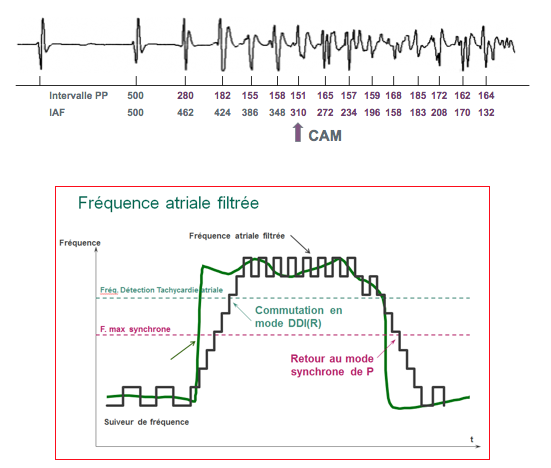
CAM uses a filtered, rather than instantaneous, atrial rate, based on a comparison of the current atrial rate with a continuously updated average rate, in order to distinguish between sustained tachycardia and rapid intermittent cycles.
When the filtered atrial rate exceeds the programmed FDTA value, the device switches to DDI(R) or VVI(R) mode.
At each cycle, the device measures the instantaneous PP interval.
It calculates a filtered atrial interval (FAI) according to the following rule:
- If instantaneous PP ≤ FAI: FAI decremented by 38 ms
- If instantaneous PP > FAI: FAI incremented by 25 ms
Mode switching occurs as soon as the filtered atrial interval falls below the atrial tachycardia detection interval.
During mode switching, the pacing frequency corresponds to the AMS base frequency (independently programmable) or to the frequency indicated by the sensor (slaved frequency).
A return to synchronous mode is only possible if the atrial frequency falls below the maximum synchronous frequency (FAI> maximum synchronous frequency interval).
Example: atrial tachycardia detection interval at 180 min-1 / 333 ms
Programming
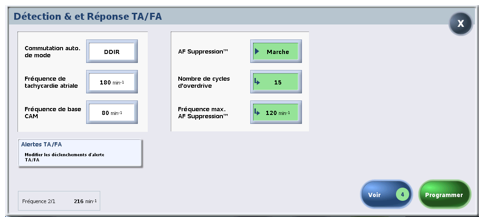
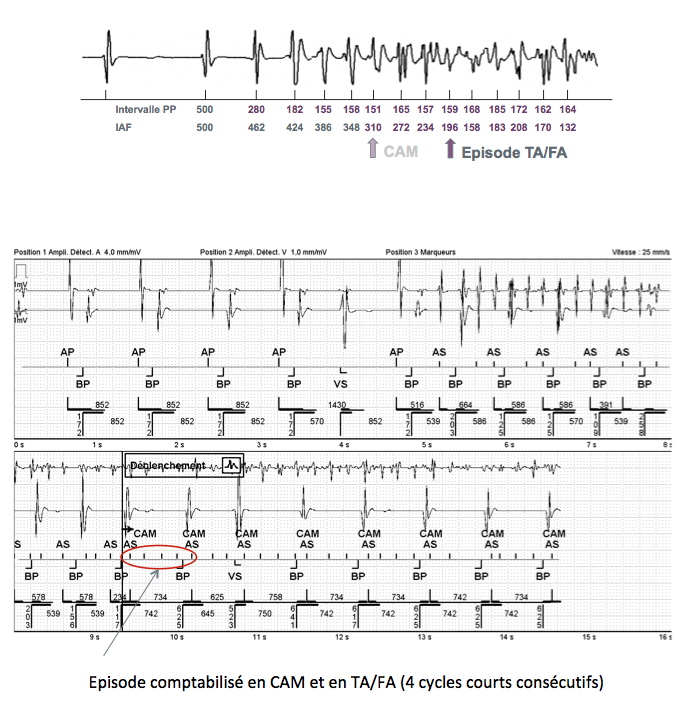
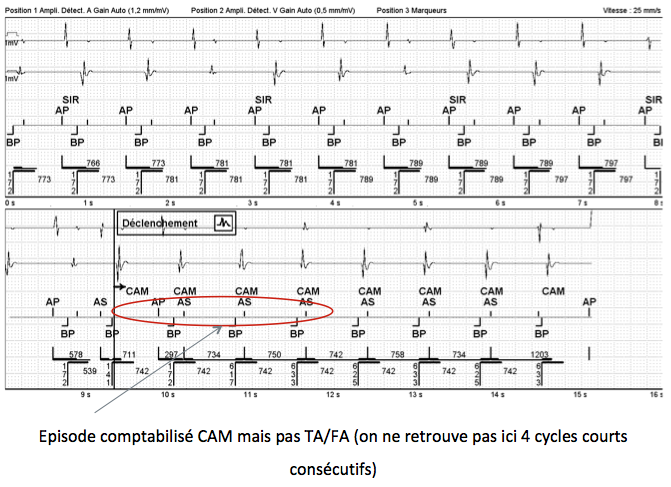
Recording a TA/FA episode
The criterion for recording AT/AF episodes is the atrial tachycardia detection interval (ATDI). The calculation method for the filtered atrial interval (FAI) is identical.
To record an episode, 4 consecutive cycles with a PP interval and a FAI that are less than the ATDI are required. These consecutive cycles make it possible to avoid the recording of AMS episodes on cross-listening (alternating short and long cycles which can lead to AMS but not to the recording of the episode because there are no consecutive short cycles). The AMS criterion is more sensitive than the recording criterion, which is more specific. 8 cycles with a PP interval and FAI greater than ATDI are then required for the episode to be completed (2 episodes less than 20 seconds apart are considered a single AT/AF episode).
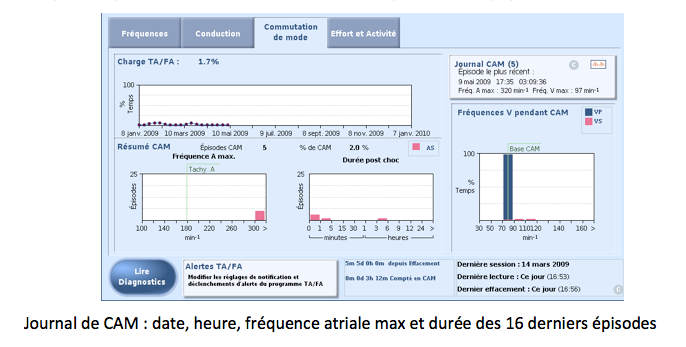
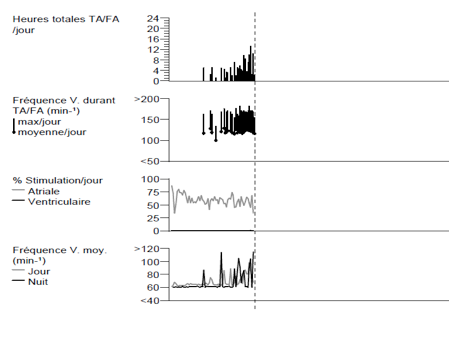
AF load
AT/AF Load is the percentage of time spent in AT/AF over a 52-week period. Each data point on the graph corresponds to the percentage of time the patient was in AT/AF over a seven-day period.
Biotronik
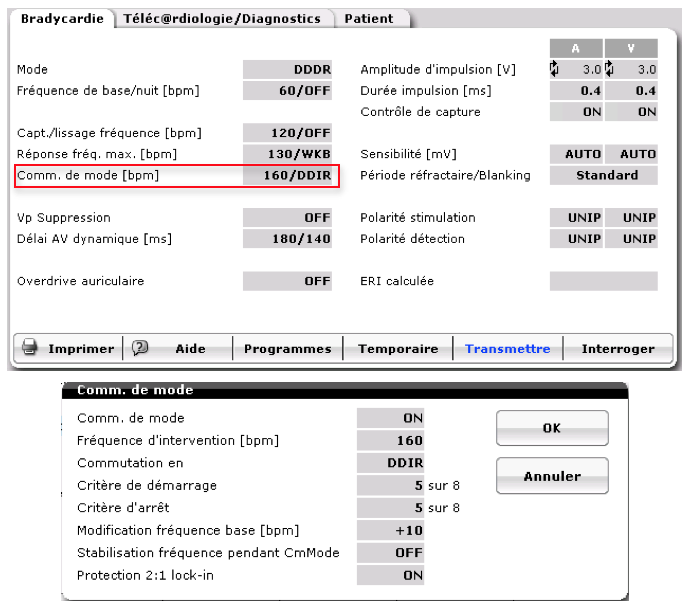
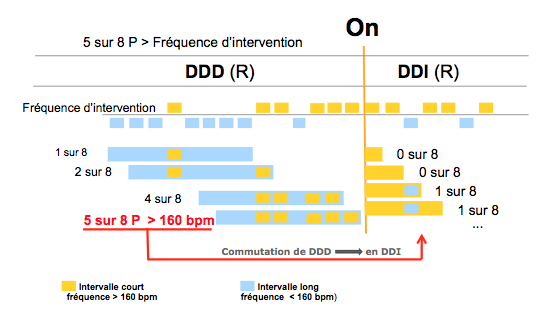
Programming the mode switch algorithm
In a Biotronik dual-chamber stimulator, various parameters of the mode switch algorithm can be programmed:
- the mode switch algorithm is programmable on or off
- the intervention frequency corresponds to the minimum atrial frequency at which the mode switch algorithm is triggered (programmable between 100 and 250 bpm, nominal value 160 bpm)
- the “switch to” corresponds to the mode in which the pacemaker retreats; it depends on the pacing mode programmed (DDD: DDI or DDIR; DDDR: DDIR; VDD: VDI or VDIR; VDDR : VDIR)
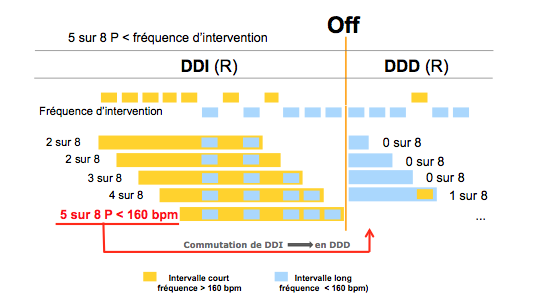
- the start-up criterion (synchronous mode to asynchronous mode) uses a rolling window of X (programmable between 3 and 8, nominal value 5) cycles out of 8; X cycles out of 8 faster than the intervention frequency are therefore required to switch to asynchronous mode; the value 5 out of 8 avoids unnecessary mode oscillations in the event of atrial extrasystoles or unstable atrial signals; similarly, it avoids inappropriate cross-listening switching when the heart rate is not fast (1 cycle out of 2 fast : 4/8)
- the stop criterion (asynchronous mode to synchronous mode) uses a rolling window of X (programmable between 3 and 8, nominal value 5) cycles out of 8; X cycles out of 8 slower than the intervention frequency are therefore required to return to synchronous mode
- modification of basal rate: a higher basal rate (programmable between 0 and 30 bpm faster, nominal value 10 bpm) can be set during mode switching to alleviate the adverse hemodynamic conditions associated with atrial arrhythmia
Querying statistics in device memories
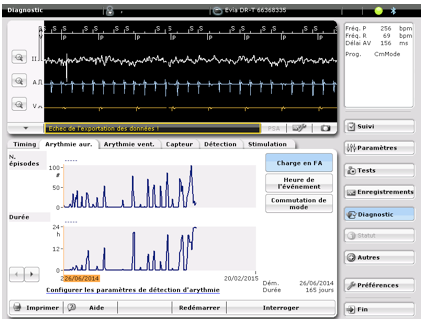
AF load
AF load is the percentage of time the patient is in AF over the course of a day. The device records the number and duration of atrial arrhythmia episodes per day for the 240 days preceding the query. For the device to record an episode, the fast atrial rate parameter must be on, and the criterion 36 events out of 48 fast cycles (faster than the programmed atrial rate) must be met.
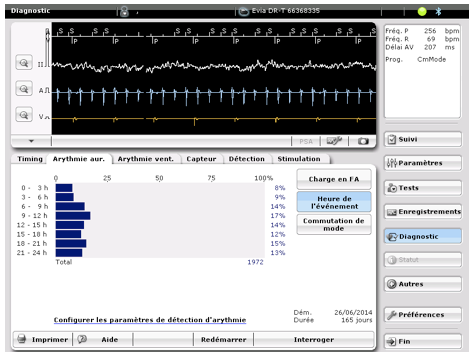
Episode timing
The device divides the day into 3-hour blocks to determine the start time of atrial arrhythmia episodes.
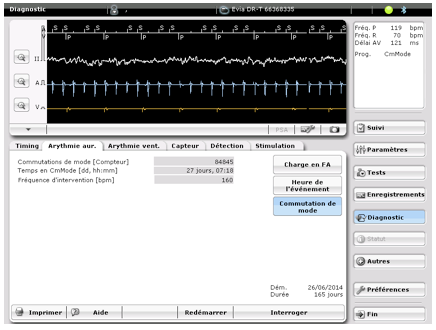
Number of mode switches
The device provides the number of mode switch episodes.
Boston Scientific
How the mode switch algorithm works
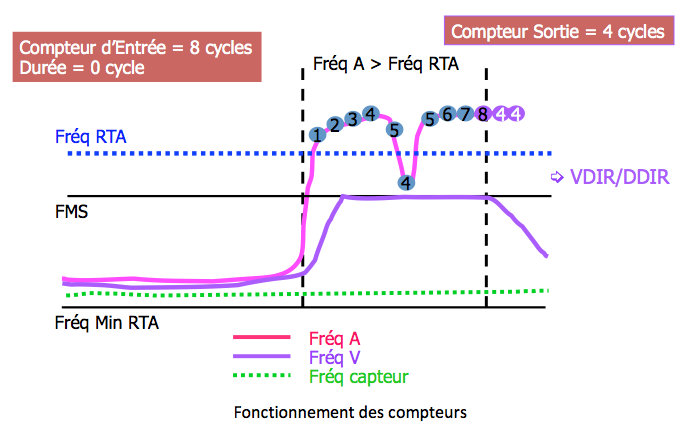
- first step: the atrial tachycardia rate is exceeded; atrial events classified as AS or in refractory period (PVARP) are included in the atrial rate calculation, unlike cycles in blankings or noise windows, which are excluded.
- second step: the input counter is completed; this counter corresponds to a number of atrial cycles faster than the fallback rate; this counter is incremented by 1 (+1) for each cycle faster than the fallback rate and decremented by 1 (-1) for each cycle detected or stimulated that is slower. When the counter is complete, the duration starts.
- third step: the duration criterion is met; the duration corresponds to the number of cycles during which the arrhythmia must persist before the mode switchover.
- fourth step: mode switchover to an asynchronous mode; this switchover starts at the end of the duration and persists until the output counter reaches 0.
- fifth step: progressive decrease in ventricular stimulation frequency; the stimulation frequency gradually decreases to reach either the programmed minimum fallback frequency or the servo frequency.
- sixth step: the output counter is completed; this counter counts atrial cycles slower than the programmed fallback frequency and starts at the time of duration; this counter is incremented by 1 (+1) for each cycle faster than or equal to the fallback frequency and decremented by 1 (-1) for each cycle detected or stimulated that is slower. If this counter reaches 0 during the duration, there is no mode switching; if this counter reaches 0 after mode switching, the device switches to a synchronous mode.
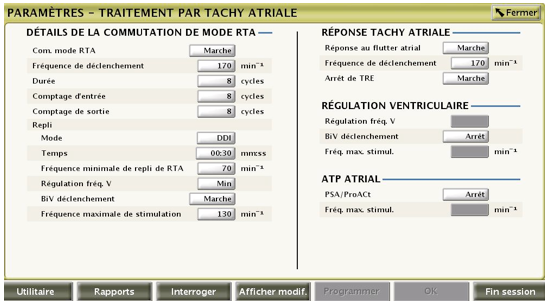
Programmable parameters
- the RTA trigger frequency corresponds to the frequency at which the device begins to detect atrial tachycardias;
- the input counter corresponds to the number of detected fast atrial events required to satisfy initial detection and activate the duration and output counter;
- the RTA duration corresponds to the number of ventricular cycles during which atrial events continue to be evaluated after initial detection; if BP persists during the duration, mode switching occurs;
- the fallback time controls how quickly the stimulated rate decreases during fallback to the minimum fallback rate or sensor rate;
Medtronic
Asynchronous mode switching (new pacemaker platform)
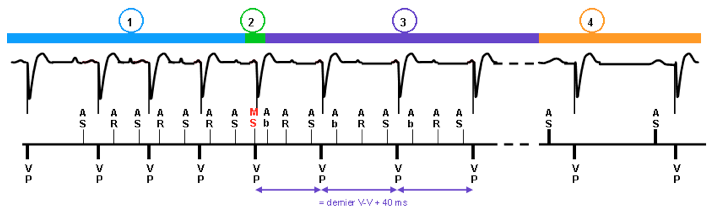
The pacemaker switches to DDIR mode (non-programmable mode) when the criterion for sudden onset of AT/AF is met, if the median value of the 12 most recent detected atrial intervals is shorter than the programmed AT/AF interval, and if the AF evidence counter (2 atrial signals detected between 2 ventricular signals) is greater than or equal to 3. To avoid an abrupt drop in ventricular rate, it very gradually reduces the pacing frequency from the synchronous atrial rate to that indicated by the sensor over several pacing cycles. Event markers include an “MS” marker for each mode switch, whether to asynchronous or synchronous mode.
- Onset of atrial arrhythmia with acceleration of stimulated ventricular rate
- Criterion for abrupt onset of AT/AF is met; MS (switch mode) marks transition to fallback; programmed pacing mode changes to DDIR mode
- Progressive transition from rapid ventricular pacing rate to servo rate (+ 40 ms at each interval)
- End of arrhythmia ; return to programmed mode (except for MVP mode, for which there is always a return to DDD before a return to AAI)
Switch to synchronous atrial tracking mode (new pacemaker platform)
The episode is stopped if a normal sinus rhythm (or normal stimulated rhythm) is identified for 5 consecutive ventricular intervals, or if the median atrial interval is greater than the AT/AF detection interval, or if the AT/AF counter is less than 27 for 3 minutes.
Memorization of atrial arrhythmia episodes
Pathological atrial events are memorized when they have generated a fold. It is possible to view the graph, EGMs and summary text for different recorded episodes.
The cardiac monitor report provides information on AT/AF episodes and ventricular rhythms, indicates the time spent in AT/AF, and provides information on the evolution of total AT/AF hours per day (graph).
Microport
Principle of the mode switch algorithm
Arrhythmia identification is based on :
- an atrial rate above which the pacemaker automatically switches to DDI mode (fallback occurs only if the atrial rate is above 120 min-1 ; this parameter cannot be modified)
- detection of abrupt atrial rhythm acceleration based on a dynamic window of prematurity = Atrial Rhythm Acceleration Detection (ARAD) window
- confirmation based on statistical processing of the atrial arrhythmia in the event of atrial under-detection
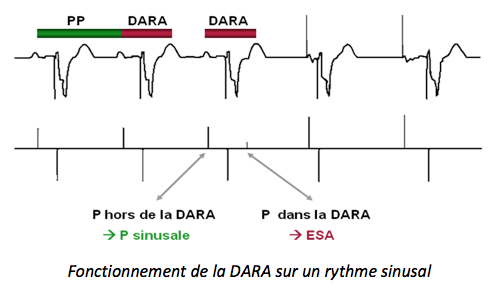
The DARA
DARA is triggered on every stimulated or detected normal atrial event. Its duration, calculated dynamically, depends on the sinus rhythm.
- when sinus rhythm is less than 80 min-1, DARA represents 62.5% of the previous P-P interval
- when sinus rhythm is greater than (or equal to) 80 min-1, DARA represents 75% of the previous P-P interval
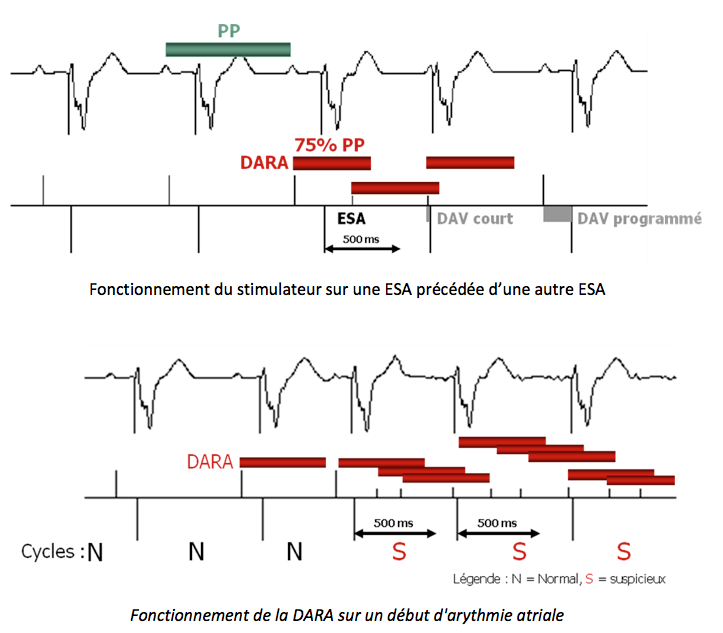
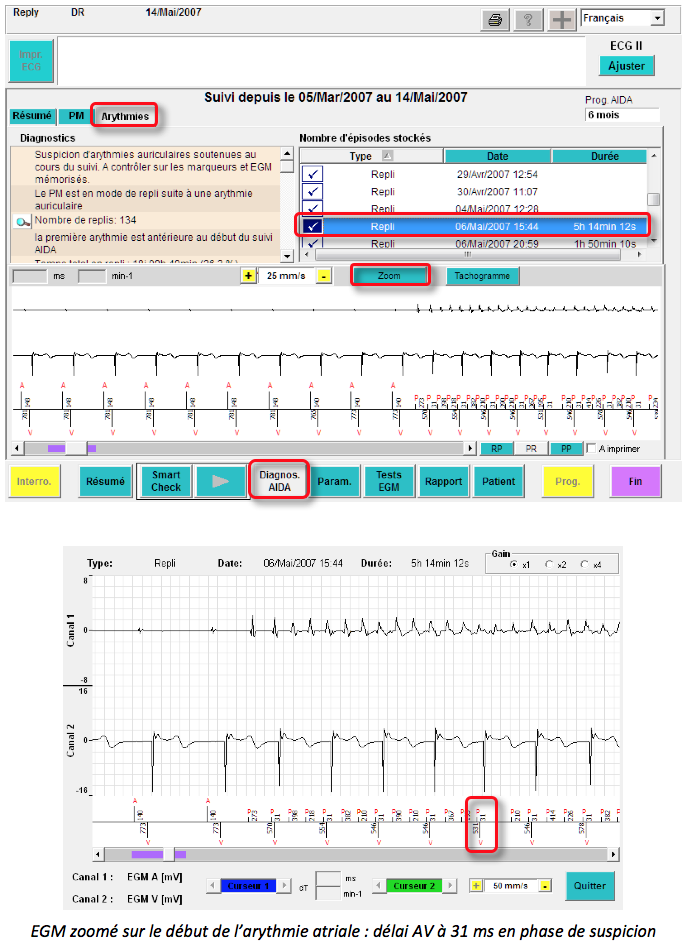
Phase of suspected atrial arrhythmia (N:1)
At the onset of rapid atrial rhythm, a short AV delay can be triggered on certain P-wave detections in DARA if, and only if, the R-V or V-V interval that would be applied is greater than 500 ms. This avoids too-rapid ventricular pacing at the start of the episode, before switching to asynchronous mode. During this phase of suspected atrial rhythm disorder, all atrial events detected are marked with refractory period markers (small “p”). The DARA value is then fixed at that of the DARA that detected the very first ESA, and may not exceed 500 ms. The short AV delay that can be triggered after certain P-wave detections in DARA is 30 ms (non-programmable).
Ventricular cycles with at least one atrial detection in the DARA window are considered “suspicious”.
How the mode switch algorithm works
The mode switch function comprises three distinct phases: a suspicion/confirmation phase, a dissociation phase and a reassociation phase.
Suspicion/confirmation phase
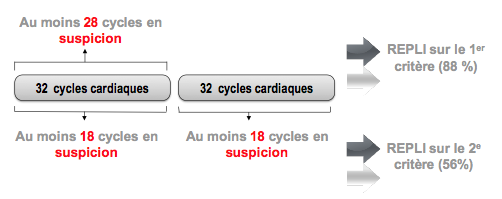
As soon as a ventricular cycle with suspected atrial arrhythmia is detected, the mode switch algorithm begins an analysis of 32 ventricular cycles (repeated per block of 32 ventricular cycles if necessary).
Atrial arrhythmia is confirmed if one of the following two criteria is met:
- 28 or more ventricular cycles are suspected during the last 32 ventricular cycles (primary criterion)
- 18 or more ventricular cycles are suspected during the last two blocks of 32 ventricular cycles (secondary criterion)
The primary criterion is usually reached in around 15 seconds. The secondary criterion may allow retreat despite atrial underdetection.
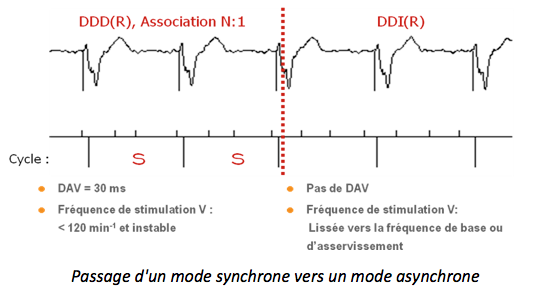
Dissociation phase
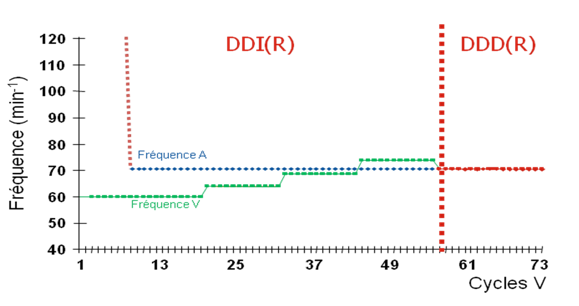
Once one of the Withdrawal criteria has been reached, the pacing mode switches from synchronous (DDD or AAI-SafeR) to asynchronous (DDI). The ventricular pacing frequency gradually decreases (the ventricular escape interval increases by 30 ms every 12 cycles) towards the base frequency, the servo frequency, or the resting frequency.
Reassociation phase
As soon as atrial arrhythmia ceases and sinus rhythm resumes, the ventricular pacing rate is gradually adapted to achieve sinus rhythm. A-V reassociation only occurs if atrial and ventricular rates are slower than 110 min-1. A 500 ms RetroPwatch is applied to the first reassociated ventricle to avoid the onset of an ERT.
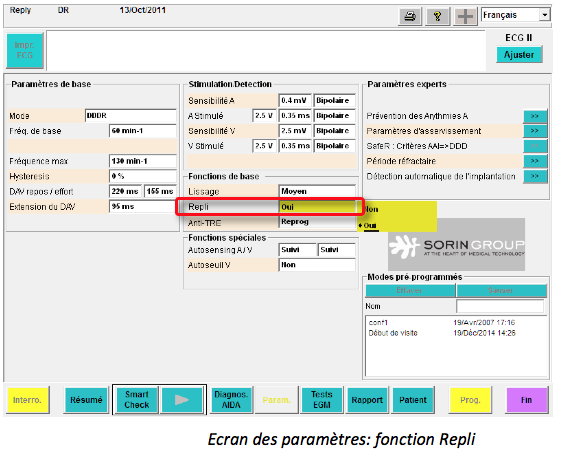
Mode switch programming
This function is activated by default.
Memory queries
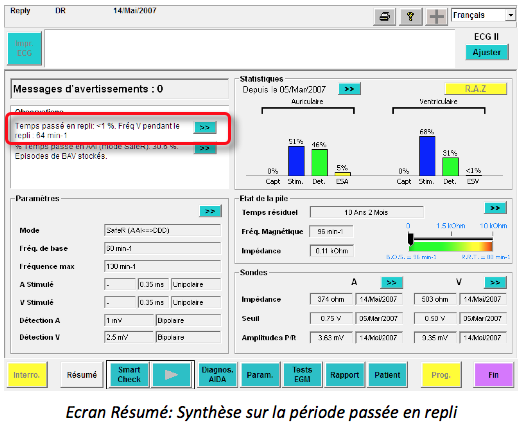
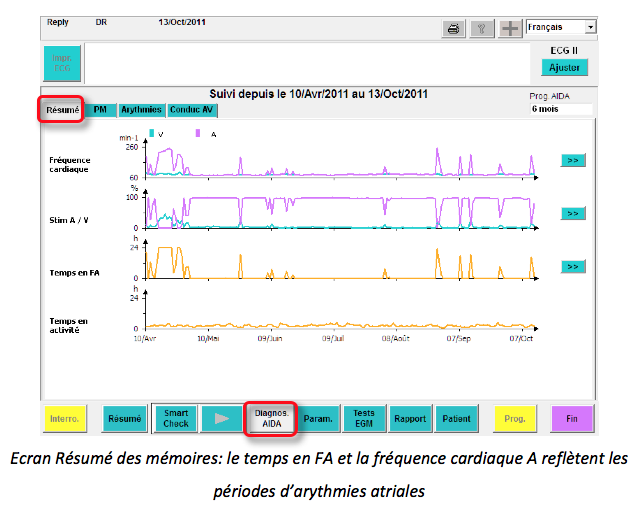
From the Summary screen, an observation is noted indicating:
Time spent in retreat (in %)
Ventricular rate during periods in retreat
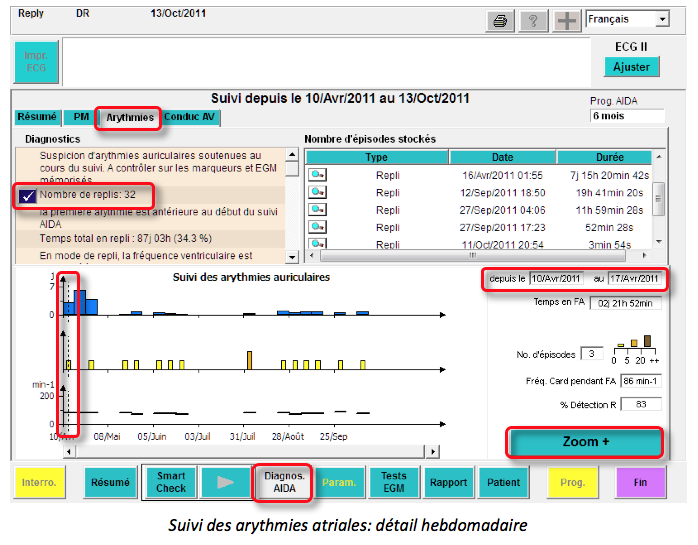
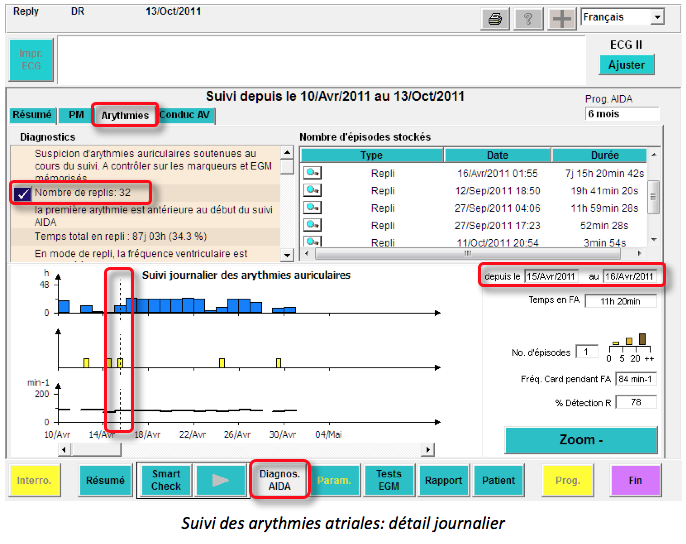
Another way to access the fallback episodes is to click on Diagnos. AIDA and then on the Arrhythmia tab.
A detailed weekly or daily view shows – duration of AF (time in fallback) – number of AF episodes – ventricular rate – percentage of ventricular detections.