Boston Scientific pacemakers in 20 points
Content
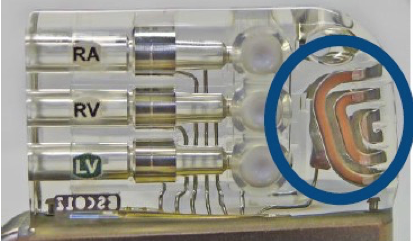
1) Case volume
Single chamber: 13.2 cm3
Double chamber: 13.7 cm3
Double chamberEL: 15.8 cm3
2) Battery type
Li/CFx Lithium-carbon monofluoride
Capacity:
- SR: 1.0 Ah
- DR: 1.0 Ah
- DR: 1.6 Ah
3) Wear and length criteria
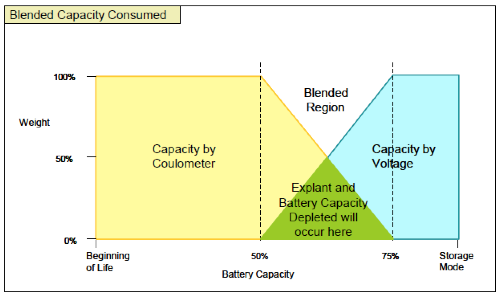
Wear criteria: the device uses a combined criterion of capacity consumed (measured by a Coulomb counter) and battery voltage to assess remaining battery life.
During the first half of the battery’s life, capacity consumed is the only criterion used, as voltage varies little and is therefore not a precise indicator. At the end of the battery’s life, however, voltage measurement offers good precision and is therefore gradually incorporated into the calculation of the estimate, until it becomes the sole criterion.
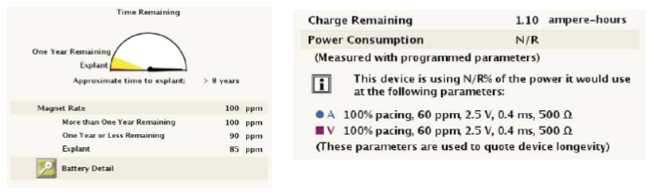
Battery gauge with various indicators:
- BOL: beginning of life
- 1 year before explantation (yellow indicator)
- Explantation (red indicator): sufficient capacity left in the battery to stimulate for 3 months at 100% under present conditions, with 1.5 hours of wireless telemetry
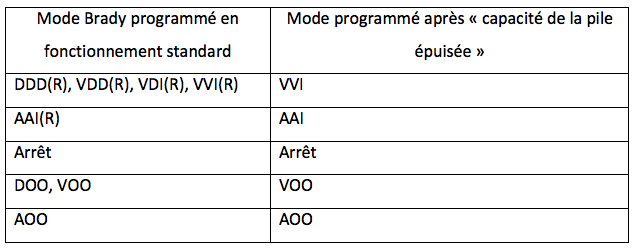
Battery capacity depleted: treatments are no longer guaranteed, and Brady mode is changed; minimum frequency is lowered to 50 min-1, RF telemetry is deactivated, parameters are no longer programmable.
If the device reaches a stage where continuous operation can no longer be guaranteed, it returns to storage mode and no functionality is available.
Data provided: approximate time to explantation, remaining capacity (Coulomb counter), power consumption
4) Magnet Frequency
One year before explantation: 90 bpm
Explantation: 85 bpm
Magnet response is programmable:
- Off: no effect of magnet application
- Store EGM: magnet application triggers 3 minutes of data storage (2 minutes before and 1 minute after): episode type, frequency and EGM. Once recording is complete (or after 60 days without magnet application), magnet mode reverts to “Stim. Asynchronous”.
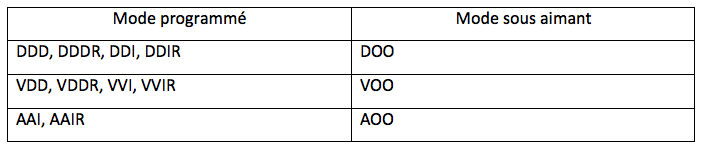
- Asynchronous stimulation: application of the magnet has the effect of converting standard Brady mode into asynchronous mode, with a fixed stimulation frequency reflecting the state of the battery and an AV delay of 100ms.
The third stimulation in the under-magnet mode is applied with pulse duration reduced by 50%. In the event of loss of capture, it may be useful to re-evaluate the programmed voltage to ensure a sufficient safety margin.
5) Traditional stimulation modes
All traditional modes are available except triggered modes.
6) Special mode for spontaneous conduction: RYTHMIQ
RYTHMIQ mode corresponds to ADI pacing mode with backup VVI at a frequency 15 bpm below the minimum frequency (cannot be slower than 30 bpm or faster than 60 bpm).
Switching AAI(R) mode with backup VVI to DDD(R) mode: if 3 slow ventricular beats are detected within an 11-beat window, the device automatically switches to DDD(R) mode. Any ventricular event detected or paced at least 150 ms below the AAI(R) pacing rate is considered a slow beat.
Switching from DDD(R) mode to AAI(R) mode with backup VVI: AV+ Search remains on AV Hysteresis for 25 cardiac cycles; if there are fewer than 2 ventricular stimulations in 10 consecutive cycles, the device automatically switches to AAI(R) pacing mode with backup VVI.
7) MRI mode
Whole body, no exclusion zone
MRI programming mode: activate MRI Protection mode (asynchronous mode) by programming the period of time after which the device automatically returns to its normal stimulation mode (12, 24, 48 hours or off).
8) Ventricular stimulation
Ventricular capture control on AUTO: PaceSafe VR
- threshold performed systematically every 21 hours
- cycle-by-cycle capture control based on evoked response analysis;
- non-programmable safety margin of + 0.5 V
- all types of unipolar or bipolar probes
- threshold measurement can be performed every 21 hours without adaptation by checking “daily trends” box
9) Atrial stimulation: no automatic measurement of atrial threshold
PaceSafe RA :
- threshold routinely measured every 21 hours;
- threshold measurement based on atrial evoked response analysis;
- no cycle-by-cycle control of capture, but adaptation for every 21 hours;
- non-programmable safety margin of 2 times the threshold (between 2V and 5V)
- bipolar probe
- possibility of measuring threshold every 21 hours without adaptation by checking “daily trends” box
10) Sensitivity and detection
Detection mode can be programmed for automatic gain control (AGC) or fixed in both atrium and ventricle. Atrial and ventricular sensitivity values can be programmed independently, with the type of detection method used (AGC or Fixed) being the same for both chambers.
If detection is set to AGC, the nominal sensitivity value is set to 0.6 mV for the ventricle and 0.25 mV for the atrium.
To optimize signal detection, the device adjusts ventricular sensitivity according to a 2-component automatic gain control: slow and fast.
11) Refractory periods
Ventricular blanking after atrial pacing is programmable, the last 40 milliseconds being the noise window (systematically retriggerable if detected). There is no safety window on Boston Scientific pacemakers.
Any event detected or stimulated in the ventricle triggers a ventricular refractory period, broken down into 2 absolute refractory periods and a noise window.
Post-detection and post-stimulation atrial refractory periods are not programmable.
Post-ventricular atrial blanking can be programmed to a fixed value or to SMART. SMART programming aims to reduce blanking times while minimizing the risk of cross-listening by suppressing the blanking period noise window and increasing the automatic gain control threshold to avoid cross-listening. Dynamic PVARP can be programmed, with PVARP decreasing linearly with heart rate.
12) Diagnosis and interruption of pacemaker mediated tachycardias
PMT detection is based on 16 consecutive AS-VP cycles occurring at maximum heart rate (not at lower rates) with stable VA intervals (+/- 32 ms). When PMT is diagnosed by the device, the PVARP is lengthened to 500 ms over one cycle.
An EGM is stored in the memories when a PMT episode is diagnosed by the device.
13) Pacemaker dependency
Boston Scientific pacemakers are equipped with 2 servo sensors that can operate separately or in combination: an accelerometer and Minute Ventilation (transthoracic impedance measurement). When the Accelerometer and Minute Ventilation sensors are both set to On for servoing, the two sensor frequencies are combined to produce a weighted average response.
14) Mode switch for atrial arrhythmias
The algorithm works in several stages: 1) the (programmable) atrial tachycardia frequency is exceeded; 2) the input counter is completed (programmable number of atrial cycles faster than the fallback frequency); this counter is incremented by 1 for each cycle faster than the fallback frequency and decremented by 1 for each cycle detected or stimulated that is slower 3) the duration criterion is met (number of ventricular cycles during which the arrhythmia must persist); 4) mode switchover to asynchronous mode; 5) output counter completed (number of atrial cycles slower than the programmed fallback frequency); this counter is incremented by 1 for each cycle faster than or equal to the fallback frequency and decremented by 1 for each cycle detected or stimulated slower; if this counter reaches 0 after a mode switchover, the device switches to synchronous mode.
15) Flutter management
The objectives of the atrial flutter response (AFR) algorithm are to prevent pacing in a vulnerable atrial period and to ensure immediate fallback in the event of an atrial frequency above the programmable AFR frequency.
16) Atrial arrhythmia prevention
3 algorithms are available
Preference to atrial pacing: increase pacing frequency to “overdrive” spontaneous atrial activation.
APP/ProACt: increase pacing rate following PAC to avoid short-cycle, long-cycle succession.
Ventricular Rate Regulation (VRR): reduce RR cycle variability by increasing the pacing percentage.
17) Wireless communication
Available on current platforms; Radio Frequency telemetry using the MICS (Medical Implant Communication Service) frequency band; dedicated medical frequency range: 402-405 MHz
18) Memory duration
Maximum EGM recording time: 14 minutes
19) Telemonitoring
Accolade compatible with the Latitude Next 3.0 System; communicator with GSM or wired transmission; yellow (programmable) and red (non-programmable) alerts triggering the sending of an e-mail or SMS with double user authentication; possibility of giving a scale and/or a blood pressure cuff connected via Bluetooth to the communicator for clinical monitoring.
20) Other features
Algorithm apnea scan: automatically detects apnea/hypopnea episodes via the decrease in respiratory volume, calculates a respiratory disorder index based on thoracic impedance measurement; identifies events when there is a 26% reduction for at least 10 seconds in respiratory amplitude (including complete pauses).