Pacemaker mediated tachycardia
Content
General information
Starting, maintaining and frequency of an PMT
Starting an PMT involves :
- programming an atrial monitoring mode (DDD or VDD)
- permeability of retrograde conduction
- momentary or permanent loss of atrio-ventricular synchronization. If ventricular activity is correctly synchronized with atrial activity, retrograde conduction is blocked.
Retrograde conduction is present in an average of 40% of patients stimulated at rest, for all indications combined. It is much more frequent in patients implanted for sinus dysfunction (up to 80%) than for atrioventricular block.
During exercise, the average incidence is 75%. These figures are sufficiently high to justify systematically programming effective protection.
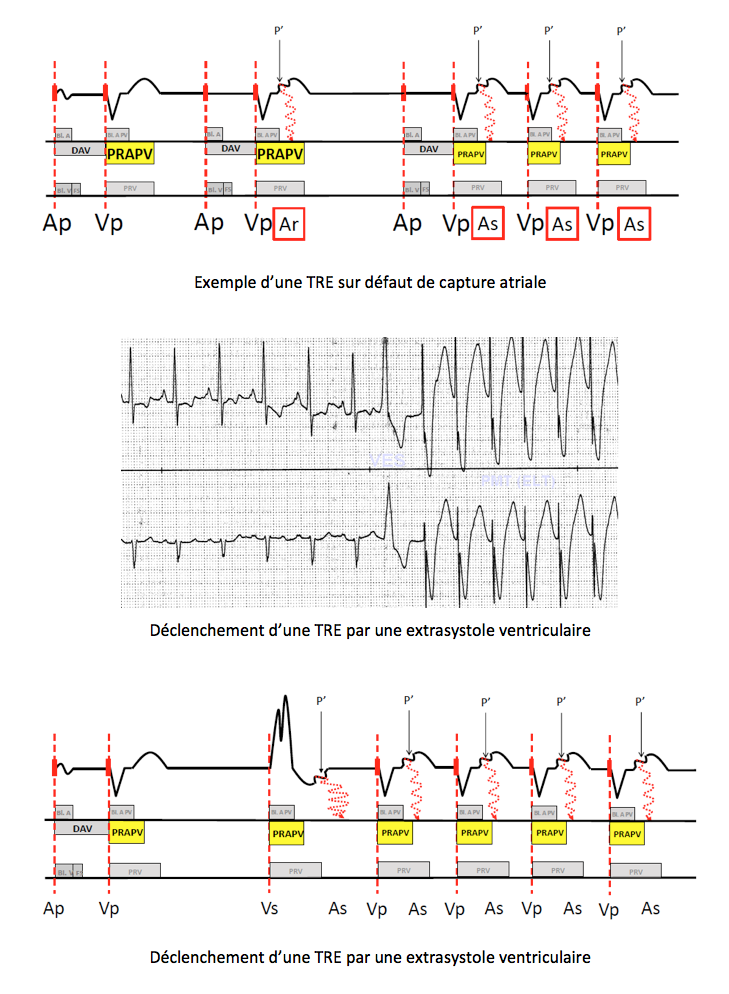
The following events may favour AV dissociation, retrograde conduction and the triggering of an PMT:
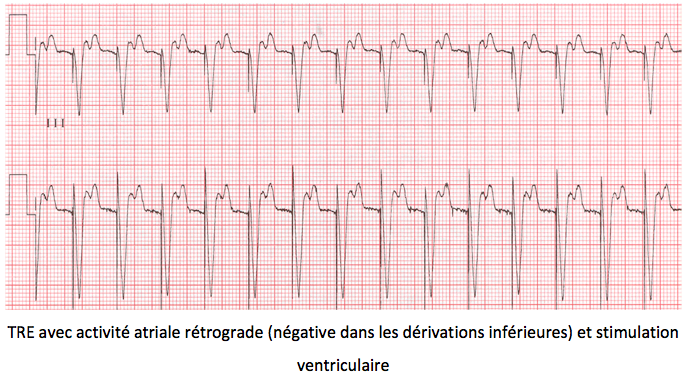
- ventricular extrasystole (most frequent cause);
atrial extrasystole with prolonged AV delay to meet - maximum programmed heart rate;
programmed AV delay too long (the nodo-hissian pathway is out of its refractory period at the time of - ventricular pacing);
external interference or myopotentials detected by the atrial chain; - a defect in atrial detection or pacing;
- a lack of PVARP extension after magnet removal, or fold exit during AV 1/1 reassociation;
- application and removal of a magnet;
- programming of VDD mode in a patient with sinus rhythm slower than the programmed minimum frequency;
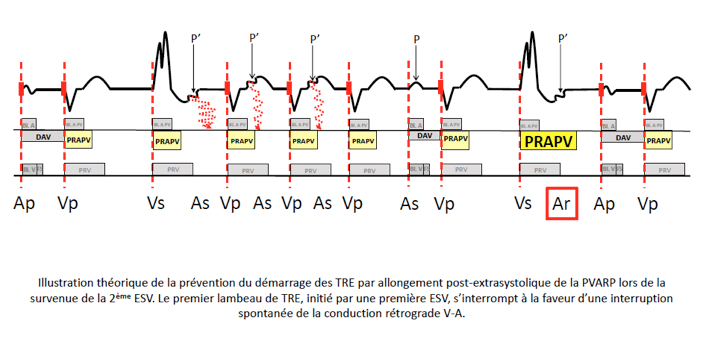
Maintenance of the PMT results from the detection, outside refractory periods, of a retrograde P’ wave, which triggers an often lengthened AV delay that favors retrograde conduction again after ventricular stimulation. An PMT is therefore a repetitive sequence in which the pacemaker reacts to each retrograde P’ wave by pacing the ventricle at a high frequency, which in turn generates a retrograde P’ wave.
The cycle repeats itself indefinitely, unless a retrograde block occurs or a specific pacemaker algorithm intervenes.
Prolonged PMT can be difficult to tolerate, with symptoms ranging from a simple feeling of discomfort or palpitations to cardiac decompensation in patients with underlying heart disease.
Heart rate during PMT depends on :
- retrograde conduction time
- programmed maximum frequency
- current AV delay
If the sum of retrograde conduction time + AV delay (at maximum frequency) is shorter than the minimum pacing interval (60000/maximum frequency), the PMT frequency is equal to the programmed maximum frequency, and the AV delay is stable and lengthened with each cycle.
If the sum of retrograde conduction time + AV delay (at PMT frequency) is longer than the minimum stimulation interval (60000/maximum frequency), the PMT frequency is lower than the maximum frequency and equal to 60000/(RCT + AV delay), and the AV delay is that programmed at the current frequency. This situation occurs in around 35% of cases.
Preventing the onset of PMT
Various complementary options can be used to prevent the onset of PMT:
- programming a mode without atrial tracking, such as DDI, to prevent the onset of PMTs. However, this pacing mode has limitations that are incompatible with the characteristics of certain patients (no monitoring of detected P waves).
- programming a PVARP longer than the retrograde conduction time that can be measured at the time of implantation. It should be borne in mind, however, that programming a PVARP that is too long can lead to the appearance of 2:1 exercise block, which is poorly tolerated by the patient. Programming an adaptable PVARP and/or AV delay increases exercise capacity. A PVARP programmed at 300 ms is sufficient in the majority of patients to avoid the onset of an PMT.
- avoid any situation favoring a loss of AV synchronism:
- program short rather than long AV delays
- ensure correct, permanent detection and pacing (sufficient margin)
- program bipolar atrial detection to avoid detection of myopotentials or external interference
automatically extend PVARP on magnet withdrawal, noise reversal output, fallback output, parameter programming - automatically extend PVARP after an PVC: the aim is to prevent tracking of retrograde P’ waves (or sinus activity) generated by ventricular extrasystoles.
- Retrograde conduction following an PVC can disrupt AV synchrony and affect pacing mode timing. The stimulator defines an PVC as any detected ventricular event that follows another stimulated, refractory or detected ventricular event without an intervening atrial event.
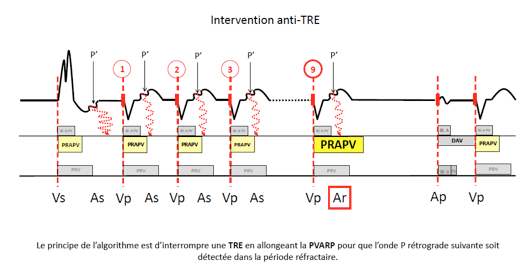
Diagnosis of an PMT by the pacemaker
The mode of diagnosis of an PMT varies from company to company, but is based on the repetition over several cycles of atrial detection and ventricular pacing with a high frequency and fixed VP-AS coupling.
PMT intervention
PMT interruption algorithms vary from manufacturer to manufacturer. Most often, once the diagnosis of PMT is suspected, the pacemaker temporarily lengthens the PVARP so that the next atrial event is detected in the refractory period. This refractory event is not synchronized to the ventricle for 1 cycle, and the tachycardia is interrupted.