Medtronic pacemakers in 20 points
Content
1) Case volume
Advisa single chamber: volume 11.9 cm3
Advisa double chamber: volume 12.7 cm3
2) Battery type
Vanadium-lithium oxide silver with carbon monofluoride
3) Wear and length criteria
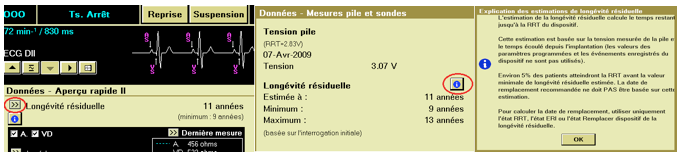
In the Quick Overview, the first value shown is the residual life. The average value is shown, as well as the minimum value. The double arrow leads to further indications, such as battery voltage, estimated service life (average, minimum and maximum) and replacement indicator. An explanation of residual life estimates is also available.
The replacement indicators are as follows:
- recommended replacement time (RRT): 3 consecutive daily automatic measurements ≤ 2.83 V. When the device reaches RRT, it continues to operate with its programmed parameters. However, placing a magnet above the device triggers asynchronous pacing at 65 min-1 rather than 85 min-1.
- Replacement indicator (ERI): 3 months after RRT. When the device reaches ERI, it automatically changes a number of parameters: pacing mode: VVI, minimum frequency: 65 min-1, single-chamber hysteresis: Off, sleep function: Off, ventricular rate stabilization: Off, AT/AF detection: Off (therapies unavailable), EGM before arrhythmia onset: Off
Note: after switching to ERI, all pacing parameters can be programmed, including mode and frequency. Reprogramming pacing parameters may shorten the period between ERI and EOS.
4) Magnet Frequency
The pacing mode is DOO when the programmed pacing mode is dual-chamber or MVP (AAIR<=>DDDR, AAI<=>DDD), VOO when the programmed pacing mode is single-chamber ventricular, and AOO when the programmed pacing mode is single-chamber atrial.
The pacing rate is 85 min-1 (700 ms) if device conditions are normal, and 65 min-1 (920 ms) if a RRT (recommended replacement time) indicator or electrical reset has occurred.
Note: this mode does not apply if telemetry between the device and the programmer is established, or if the SureScan MRI function is set to On.
5) Traditional stimulation modes
All traditional modes are available except for triggered modes and VDD mode.
6) Special mode for spontaneous conduction: Managed Ventricular Pacing (MVP mode or AAI(R)-DDD(R) )
ADI(R) è DDD(R) switching criteria: if only one P-wave is blocked, the device remains in ADI(R) mode and provides a backup ventricular pacing pulse 80 ms after the atrial escape interval. If 2 out of 4 P waves are blocked, the device switches to DDD(R) mode.
DDD(R) è ADI(R) switching criteria: when the stimulator is operating in DDD(R) mode, it searches for the presence of an underlying clean rhythm every 1 minute, then 2, 4, 8…minutes, up to a maximum of 16 hours. To do this, the device switches to ADI(R) stimulation mode for one cycle (possibility of blocked P-wave). If atrial activation is successful, it remains in ADI(R) stimulation mode, otherwise (P wave blocked) it switches back to DDD(R) mode.
7) MRI mode
Surescan MRI mode; programmable parameters include mode (ODO, VOO, DOO), frequency, AV delay, stimulation amplitudes and pulse durations; programming required before MRI and reprogramming afterwards; whole-body MRI without exclusion zone;
8) Ventricular stimulation
Right ventricular threshold control on dynamics: daily measurement of ventricular stimulation threshold + adaptation of programming for 24 hours; ventricular capture control on monitor: measurement of ventricular stimulation threshold without adaptation.
Threshold performed systematically every 24 hours at 1:00 a.m.; pacing threshold based on evoked response analysis; single daily measurement with adaptation for 24 hours; target amplitude by multiplying the VD amplitude safety margin by the amplitude threshold measured at a pulse duration of 0.4 ms within an output range defined by a programmable lower limit (Adjusted minimum amplitude parameter) and the upper threshold limit of 5.0 V and 1.0 ms. The minimum pulse duration for ventricular threshold control is 0.4 ms.
9) Atrial stimulation: no automatic measurement of atrial threshold
Dynamic atrial threshold control: daily measurement of atrial stimulation threshold + programming adaptation for 24 hours; monitor-based atrial capture control: measurement of atrial stimulation threshold without adaptation.
Threshold systematically measured every 24 hours at 1:00 a.m.; threshold measurement based on the synchronization of detected P and R waves (2 methods depending on the presence or absence of atrioventricular conduction); single daily measurement with adaptation for 24 hours; target amplitude by multiplying the OD amplitude safety margin by the threshold measured at a pulse duration of 0.4 ms within an output range defined by a programmable lower limit (Adjusted minimum amplitude parameter) and the upper threshold limit of 5.0 V and 1.0 ms. The minimum pulse duration for atrial threshold control is 0.4 ms.
10) Sensitivity and detection
On the latest stimulators, detection is automatic if programmed as bipolar (fixed if unipolar). After ventricular detection, the threshold value adjusts to 75% of the R wave (maximum 8 x the programmed value), then decreases over time (450 ms) to reach the programmed sensitivity (e.g. 0.9 mV). After atrial detection, the threshold value adjusts to 75% of the P wave (maximum 8 x programmed value), then decreases over time (200 ms) to reach the programmed sensitivity (e.g. 0.3 mV).
11) Refractory periods
Ventricular blanking after atrial pacing is non-programmable. The safety window lasts up to 110 ms after atrial pacing.
Any event detected or stimulated in the ventricle triggers a non-programmable blanking period.
If the pacemaker is programmed for MVP mode, and operates in AAI mode, the post-stimulation atrial refractory period is automatically adjusted to 75% of the cardiac cycle, up to a maximum of 600 ms.
For the latest pacemakers, the post-ventricular atrial blanking method can be programmed as absolute (traditional blanking), partial (Ab marker counted for arrhythmia diagnosis) or partial + (temporary drop in sensitivity, Ab marker counted for arrhythmia diagnosis).
PVARP can be set to a fixed value or automatic.
12) Diagnosis and interruption of pacemaker mediated tachycardias
The PMT intervention algorithm is OFF in nominal mode. It must therefore be programmed systematically.
The stimulator defines the occurrence of a PMT when it detects a ninth ventricular stimulation following eight consecutive VA intervals with a VA interval of less than 400 ms. Sensor analysis allows differentiation between sinus tachycardias.
The PMT is stopped by lengthening the PVARP to 400 ms.
After an intervention, the anti-PMT intervention function is automatically suspended for 90 seconds.
No EGM recording of PMT episodes in memory.
13) Pacemaker dependency
Frequency feedback is based on data supplied by an accelerometer.
Independent servo control is provided in two frequency ranges: AQ (daily activity) and intense effort. The optimization system acts on the slope adjusting the linear relationship in both frequency ranges.
14) Mode switch for atrial arrhythmias
The pacemaker switches to DDIR mode (non-programmable mode) if the median value of the 12 most recent detected atrial intervals is shorter than the programmed AT/AF interval, and if the AF evidence counter (2 atrial signals detected between 2 ventricular signals) is greater than or equal to 3.
Episode termination and return to synchronous mode occur following identification of normal sinus rhythm (or normal stimulated rhythm) for 5 consecutive ventricular intervals, or if the median atrial interval is greater than the AT/AF detection interval, or if the AT/AF counter is less than 27 for 3 minutes.
15) Flutter management
The masked flutter search algorithm looks for the presence of an atrial signal that has not been seen because it falls into atrial blanking post ventricular pacing, by extending the PVARP over one cycle (no ventricular pacing and detection of hidden atrial activity).
The specificities of blanking on the new platforms (signal counted for arrhythmia diagnosis) limit the interest of this type of algorithm.
16) Atrial arrhythmia prevention
5 algorithms are available
Non-competitive atrial pacing: avoid triggering an atrial arrhythmia by pacing during the relative atrial refractory period.
Atrial pacing preference: increase pacing frequency to “overdrive” spontaneous atrial activation.
Stabilization of atrial rhythm: increase pacing frequency following PAC to avoid short-cycle, long-cycle succession.
Rapid post-mode-switching pacing: rapid atrial pacing immediately after a mode-switching episode.
Response to controlled AF: reduce RR cycle variability by increasing the percentage of pacing.
17) Wireless communication
Technology currently unavailable
18) Memory duration
Maximum EGM recording time: 24.5 minutes (5 min TV episodes, 2 min TVNS, 8.25 min treated AT/AF episodes, 3 min recorded TA/FA episodes, 2 min double tachycardias, 2.5min supraventricular episodes, 1.75 min patient activation).
There is also a flashback memory: recording of the 2000 atrial and ventricular intervals preceding tachyarrhythmia episodes or the most recent interrogation.
19) Telemonitoring
No automatic transmission or on alerts. Manual transmission is possible.
20) Other features
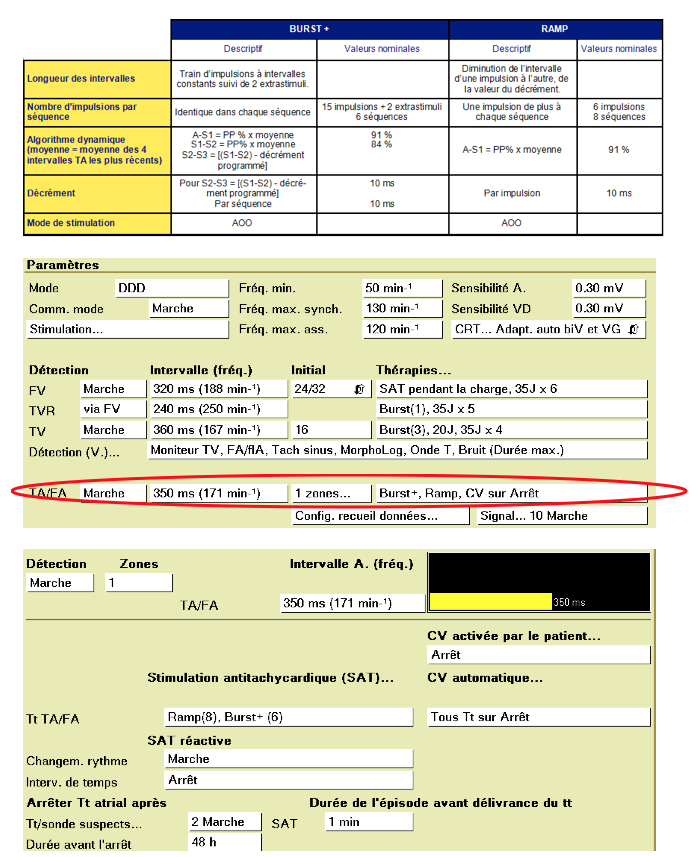
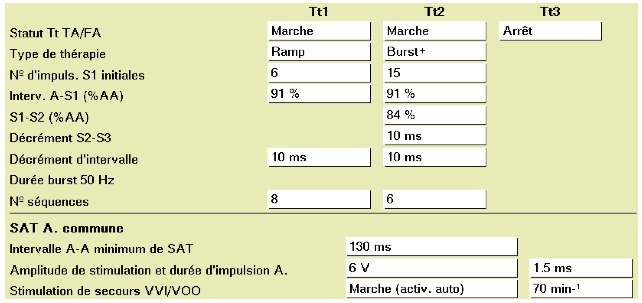
Programmable therapies to treat atrial arrhythmia episodes;
The device can deliver up to 3 ATP therapies to treat AT/AF or a rapid AT/AF episode. These therapies correspond to Burst + or Ramp, each with a programmable number of sequences. All ATP therapies are delivered in AOO mode, however, VVI/VOO pacing is available when atrial ATP therapies are delivered.