General AV delay and refractory periods
Content
1. Atrioventricular delay
In a dual-chamber pacemaker, the AV delay determines the maximum time interval between an atrial event and the expected delivery of ventricular pacing. This interval corresponds to the electronic equivalent of the PR interval.
There are separate AV delays for paced and sensed atrial events.
These are programmed to ensure perfect mechanical coordination between atria and ventricles, whether the atrium is sensed or stimulated. The length of these intervals can be programmed over a wide range, fixed or adaptive, and is influenced by a large number of algorithms.
Stimulated AV delay
The stimulated AV delay is applied following atrial stimulation when the stimulator is operating in DDD, DDI, DVI and DOO modes.
Detected AV delay
Detected AV delay is applied following a detected atrial event when the stimulator is operating in atrial synchronized pacing mode (DDD and VDD).
Setting the AV delay
The AV delay that results in optimal hemodynamics varies considerably from patient to patient. Precise adjustment of the AV delay should ensure that the temporal relationship between left atrium and left ventricle remains constant, and that left atrial systole is completed before the onset of left ventricular systole.
Permanent programming of long AV delays (increased risk of PMT and pacing in a vulnerable period of undetected ESV in post-atrial ventricular blanking, poor hemodynamic results with E-wave and A-wave fusion) in non-dependent patients to promote spontaneous conduction can be avoided today thanks to the use of specific modes previously described (MVP, AAI-SafeR…).
If the patient is dependent (complete atrioventricular block), the mean value of the optimal detected AV delay at rest is around 110 ms.
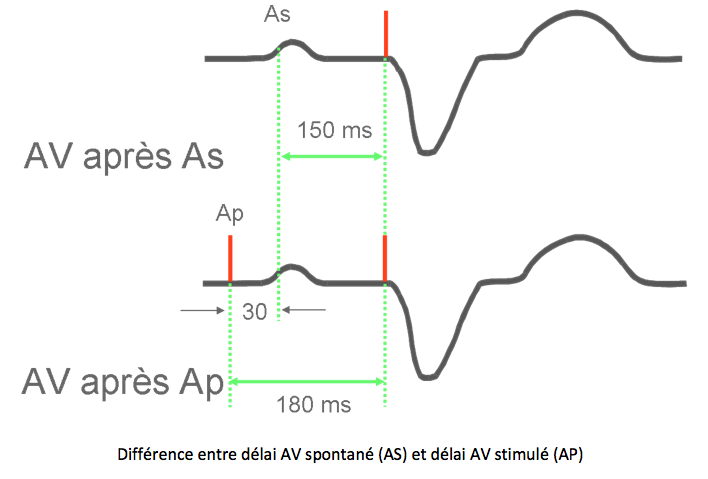
Difference between stimulated and detected AV delays
The optimal detected AV delay is shorter than the optimal stimulated AV delay for a number of reasons:
- the P wave is never detected at the very start of the surface P wave, but when the atrial depolarization wave passes under the electrode. This is often later than the onset of the P wave on the surface ECG.
- when the P wave is stimulated, the conduction time between the right and left atria is lengthened.
- the difference between detected and stimulated AV delays depends on the position of the probe in the right atrium: on average 30 ms if the probe is inter-atrial septal, 50 ms if it is in the atrium, 70 ms at the high part of the right atrial border and 90 ms if it is lateral low. These values are averages, and in theory programming should be adapted to each individual. These differences are often longer if there is an intra- and/or inter-atrial conductive disorder.
- this difference changes little with effort, with a tendency to shortening under the influence of catecholamines, which reduce inter-atrial conduction time. If there is a major inter-atrial conductive disorder, this difference may increase with exercise. In practice, this value can remain fixed throughout the programmed frequency variation range.
Adaptable AV delay
Physiologically, the PR interval shortens during exercise, on average by 4 ms for every 10 beats of acceleration in frequency. AV delay adaptation is designed to reproduce this physiological phenomenon, and the same variation is applied to the detected AV delay as to the stimulated AV delay.
The specifics of adaptable AV delay will be dealt with in the chapter on stress tuning.
2. Refractory periods during inhibited (DDI) or triggered (DDD) modes
Refractory periods of a single-chamber pacemaker
The refractory period is an interval following pacing or detection of an event in the implanted cavity, during which the pacemaker, operating in inhibited (SSI) or triggered (SST) mode, is not recycled.
On a stimulator operating in VVI mode, the first part of the refractory period is a programmable blanking period. This refractory period ensures that the pacemaker is not recycled on ventricular pacing afterpotential detection and repolarization T-wave detection.
The refractory period is generally set at between 220 and 350 ms.
A value set too short encourages over-detection, resulting in recycling of the escape interval and a drop in pacing rate. If the programmed value is too long, ventricular extrasystoles may be missed and fall into the refractory period. In this case, at the end of the pacing interval, there is a risk of a stimulus appearing in the T wave of the extrasystole.
On a pacemaker operating in AAI mode, the first part of the refractory period is a programmable blanking period. The refractory period must avoid recycling by an R wave seen in the atrium (ventriculo-atrial cross-talk). Its value should cover the AR interval (between atrial stimulus and R wave), which is longer than the PR interval. However, it must not be too long to ensure atrial detection up to the maximum frequency controlled by the sensors.
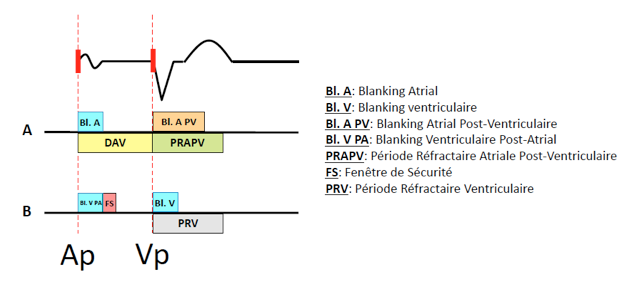
Refractory periods of a dual-chamber pacemaker
Atrial or ventricular pacing initiates different blankings or refractory periods in the cavity under consideration, but also in the other cavity to avoid cross-tapping.
Two types of refractory periods are set up:
- blanking periods deactivate detection for a programmable or non-programmable interval, and protect against:
- post-stimulation potentials in each chamber;
- atrio-ventricular or ventriculo-atrial cross-listening;
- refractory periods where detected events are taken into account for arrhythmia diagnosis and for the operation of various algorithms, but do not recycle certain synchronization intervals.
Refractory periods are designed to prevent certain synchronization intervals from being recycled by the detection of incorrect signals such as retrograde P-waves, distant R-waves or electrical interference.