Biotronik pacemakers in 20 points
Content
1) Case volume
Single chamber: 11 cm3
Double chamber: 12 cm3
2) Battery type
Lithium/Manganese Dioxide or Lithium/Silver/Vanadium Oxide
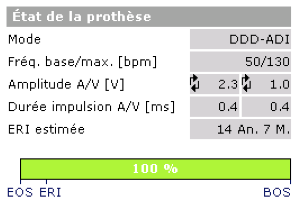
3) Wear and length criteria
Values shown: estimated ERI date and residual battery charge in %.
ERI operation: switch to a mode without atrial pacing or servo control (e.g. DDDR->VDD), frequency reduced by 11%; ERI lasts 6 months before switching to EOS.
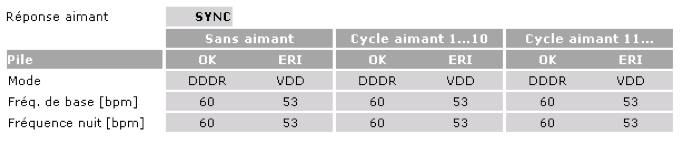
4) Magnet Frequency
Early life: 90 bpm
End of life: 80 bpm
3 options for magnet response can be programmed: Sync, Async and Auto
5) Traditional stimulation modes
All traditional modes are available.
6) Special mode for spontaneous conduction: VP suppression
ADI(R) è DDD(R) switching criteria: various criteria lead to switching to DDD mode: pause (2 second interval without VS), AVB III (2 consecutive cycles without VS), AVB II (3 (programmable) cycles out of 8 without VS), AVB I (PR or AR > 450 ms over 2 cycles).
Suspension of Vp Suppression for 20 hours in the event of numerous (15) switches from one mode to another. The stimulator remains in DDD temporarily.
DDD(R) è ADI(R) switching criteria: when the stimulator is operating in DDD mode, it searches for the presence of an underlying clean rhythm every 30 seconds, then intervals the search (every 1, 2, 4, 8, 16…128 minutes, up to 20 hours). To do this, the stimulator extends its AV delay to a value of 450 ms for 8 cycles. The stimulator switches to ADI mode if 1 spontaneous ventricle is detected during this extended AV delay on at least 6 of these 8 cycles.
7) MRI mode
Thoracic exclusion zone for the first MRI-compatible stimulators; no exclusion zone for the latest generation (Evia platform marketed from 2013 combined with Solia screw probes);
Choice of MRI mode: DOO, VOO, AOO, OOO;
MRI mode must be programmed before and reprogrammed after examination. The programmer recognizes the MRI-specific programming and automatically proposes to transmit the initial programming.
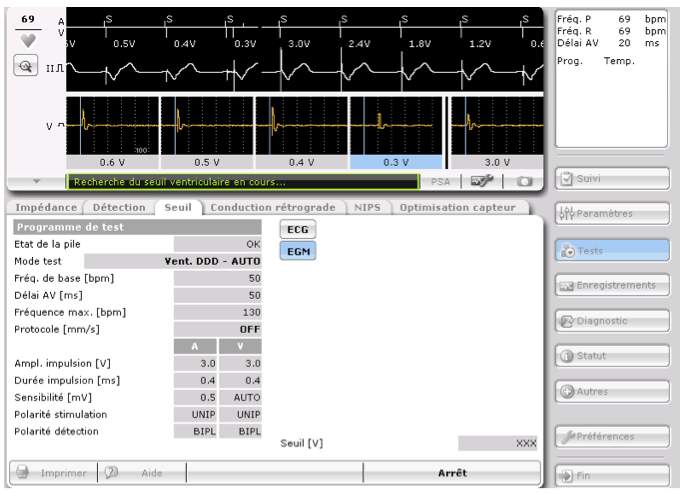
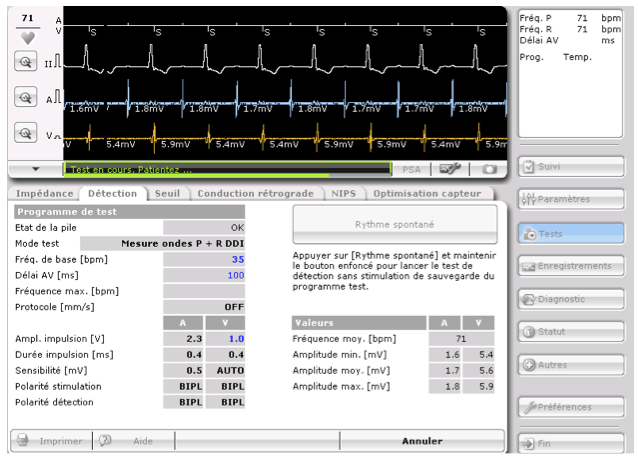
8) Ventricular stimulation: ventricular capture control
On-run ventricular capture control: ventricular stimulation threshold measurement + programming adaptation with cycle-by-cycle control; ATM ventricular capture control: ventricular stimulation threshold measurement without adaptation;
Threshold systematically measured every day at 2:00 a.m. (programmable control time and frequency); capture control based on evoked response analysis; cycle-by-cycle capture verification; programmable safety margin (nominal value + 0.5 V).
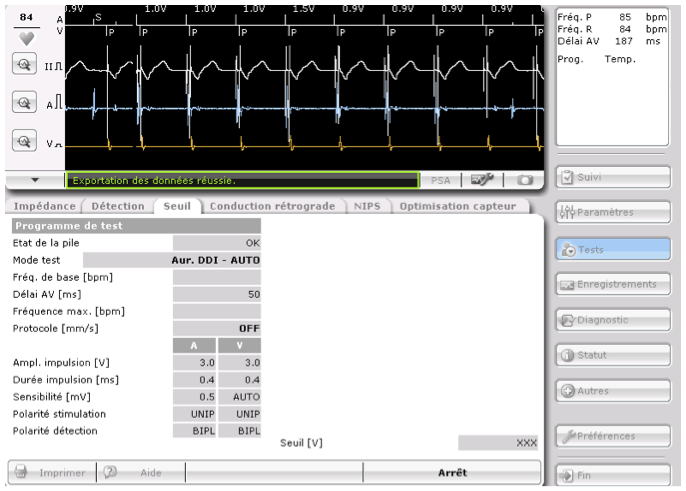
9) Atrial stimulation: no automatic measurement of atrial threshold
Atrial capture control on walk: measurement of atrial stimulation threshold + adaptation of programming; atrial capture control on ATM: measurement of atrial stimulation threshold without adaptation;
Threshold performed systematically every day at 2:00 a.m.; atrial stimulation threshold based on detected atrial signals indicative of loss of capture; no cycle-by-cycle verification of capture; amplitude adaptation for 24 hours; programmable safety margin (nominal value + 1 V).
10) Sensitivity and detection
Atrial and ventricular sensitivities can be programmed to a fixed value or with automatic adaptation (automatic sensitivity control). Automatic sensitivity control measures the size of the R or P wave and adapts the sensitivity threshold cycle by cycle.
The maximum automatic sensitivity is 2 mV for ventricular detection, 0.2 mV for bipolar atrial detection and 0.5 mV for unipolar atrial detection.
11) Refractory periods
Post-atrial stimulation ventricular blanking is programmable between 30 and 70 ms (nominal value 30 ms). At the end of this blanking period, the non-programmable safety window begins (ending 100 ms after atrial pacing).
Any event detected or stimulated in the ventricle triggers a programmable ventricular refractory period.
The atrial refractory period occurs following a stimulated or detected atrial event when not in refractory period (programmable to a fixed value or Auto).
Post-ventricular atrial blanking (far-field protection) is programmable. If an event falls within this blanking, it is noted Ars (FFP) but does not trigger an AV delay and is not counted for the diagnosis of atrial arrhythmias. The Post-Ventricular Atrial Refractory Period (PVARP) is triggered only by ventricular pacing and not by ventricular sensing (VS). It is also triggered by ventricular extrasystole. PVARP can be set to Auto or to a fixed value.
12) Diagnosis and interruption of pacemaker mediated tachycardias
One of the special features of Biotronik pacemakers is the ability to measure retrograde conduction time to adapt PVARP programming.
The device suspects the existence of an RTC if the heart rate exceeds 100 beats/minute, with a succession of 8 consecutive VP-AS cycles, if the VA interval (VP-AS) is shorter than the programmed VA interval, and if the VA intervals are stable (+/-25 ms).
To confirm the PMT, the AV delay is increased or decreased; if the VA interval remains constant : PMT; reduction of PMT: lengthening of PVARP.
No EGM recording of PMT episodes in memory.
13) Pacemaker dependency
Rate control can be based on an accelerometer or on a specific mode known as CLS (closed loop stimulation); these 2 sensors operate independently and cannot be programmed simultaneously. CLS (closed loop stimulation) is based on heart rate adaptation targeting impedance variations that follow the dynamics of myocardial contraction. Closed-loop stimulation calibrates and adapts automatically. It enables adaptation to both physical and mental effort.
14) Mode switch for atrial arrhythmias
The fallback algorithm uses a rolling window of X (programmable between 3 and 8, nominal value 5) cycles out of 8 above the intervention frequency to switch to asynchronous mode. The algorithm also uses a rolling window of X (programmable between 3 and 8, nominal value 5) cycles out of 8 below the intervention frequency to return to synchronous mode.
15) Flutter management
The 2:1 lock in protection algorithm (lengthening the AV delay to reveal atrial activity hidden in far-field protection) enables switching when every other atrial activity falls into far-field atrial protection post ventricular pacing.
16) Atrial arrhythmia prevention
2 algorithms are available: atrial overdrive, which increases the atrial pacing frequency to “overdrive” spontaneous atrial activation; frequency stabilization, which reduces RR cycle variability by increasing the pacing percentage.
17) Wireless communication
Technology not available on current platforms
Technology available on next-generation platforms
18) Memory duration
Maximum EGM recording time: 20 x 10-second episodes
19) Telemonitoring
Automatic system without patient intervention; integrated GPRS; daily transmissions of all overnight measurements, settings, long-term trends; event notifications within 24 hours (atrial load, high ventricular rate episode, out-of-range impedance …); periodic 30-second EGMs; remotely sent arrhythmia iEGMs (AF, VT, …), available on next generation.
20) Other features
Exceptional experience in telemedicine