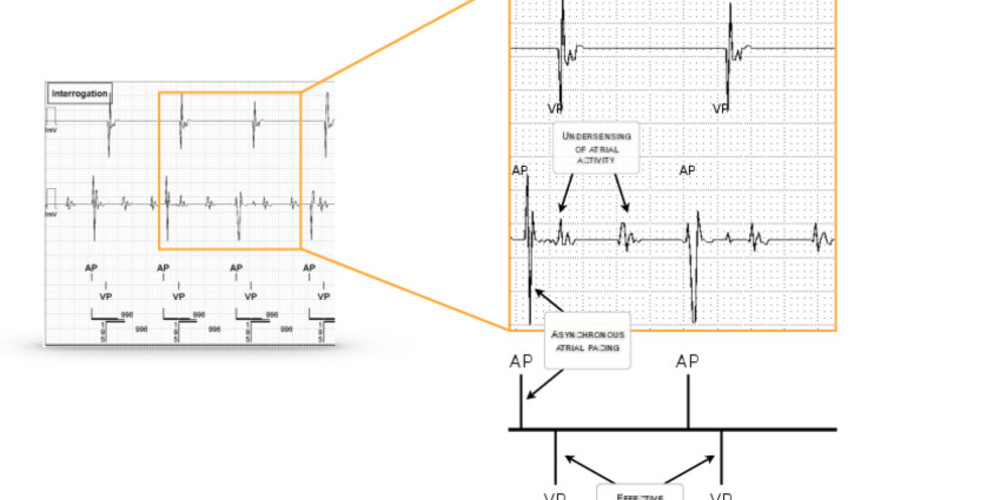
atrial sensing failure
Tracing
Manufacturer Abbott
Device PM
N° 22
Patient
A 69-year-old woman with history of infarction implanted with an AssurityTM + DR pacemaker for complete atrioventricular block; episodes of paroxysmal AF.

Graph and trace
Programming in DDD mode 60 beats/minute; atrial arrhythmia undetected; asynchronous atrial pacing followed by effective ventricular pacing.
Other articles that may be of interest to you





These tracings show atrial undersensing in a patient with AF followed by sinus rhythm. The sensing of the P wave presents certain peculiarities, with the slope of the signal and its amplitude being lower than those of a QRS complex. In addition, the amplitude of the sensed atrial signal can vary depending on the position of the patient and the respiratory cycle. It is therefore important to program a sufficient margin to avoid atrial undersensing problems during exercise which can cause a sudden decrease in the ventricular pacing rate in a patient with atrioventricular block. In addition to the lack of proper P wave monitoring during exercise, atrial undersensing can also have a proarrhythmogenic effect if atrial pacing occurs during a vulnerable atrial period with a risk of induction of atrial arrhythmia. In this patient, undersensing of atrial arrhythmia is responsible for inefficient and unnecessary atrial pacing thereby increasing energy consumption and reducing battery performance. Atrial arrhythmias are not counted thus skewing the data in terms of arrhythmia load rendering the device memory unreliable for assessing the efficacy of antiarrhythmic therapy or for initiating anticoagulant therapy. The second tracing shows an undersensing of sinus activity also leading to the occurrence of asynchronous atrial pacing. In a patient with premature ventricular contractions, as in this tracing, the risk is the occurrence of the undetected extrasystole since falling within the post-atrial ventricular blanking period with potentially-arrhythmogenic ventricular pacing at the end of the programmed AV delay.
When adaptive atrial sensitivity is programmed, after sensing of an atrial signal, the sensitivity adjustment level begins at a programmable percentage of the sensed signal amplitude (not exceeding 3 mV nor falling below 0.3 mV), remains the same during the decay delay (programmable) after which the sensitivity gradually increases until reaching the programmed sensitivity value. The following parameters are programmable: the post-sensed adjustment level (threshold start between 50 and 100%), the post-paced adjustment level (between 0.2 and 3 mV), the post-sensed decay delay (between 0 and 220 ms), the post-paced decay delay (between 0 and 220 ms) and the maximum sensitivity (between 0.2 mV and 1 mV).