Microport - Atrial arrhythmia management
Content
Mode-switch algorithm
Principle of the mode-switch algorithm
Arrhythmia identification is based on:
- an atrial rate above which the pacemaker automatically switches to DDI mode (fallback only occurs if the atrial rate exceeds 120 min-1; this parameter cannot be modified)
- detection of a sudden acceleration in atrial rhythm based on a dynamic prematurity window = Atrial Rhythm Acceleration Detection (WARAD)
- confirmation based on statistical processing of atrial arrhythmia in the event of atrial under-detection
WARAD
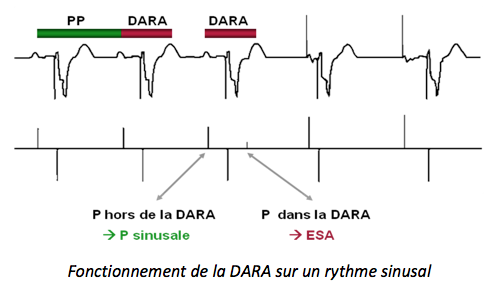
WARAD is triggered on each stimulated or detected normal atrial event. Its duration, calculated dynamically, depends on the sinus rate.
When the sinus rhythm is less than 80 min-1, WARAD represents 62.5% of the previous P-P interval
When the sinus rhythm is greater than (or equal to) 80 min-1, WARAD represents 75% of the previous P-P interval
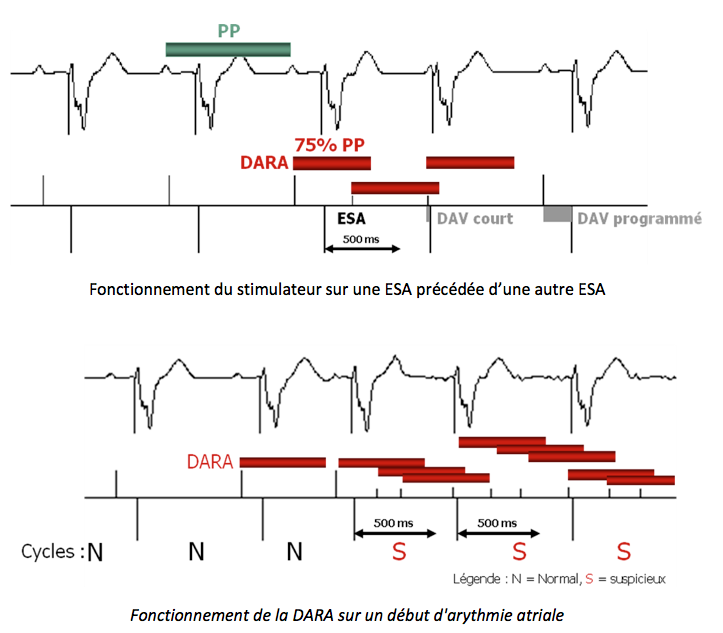
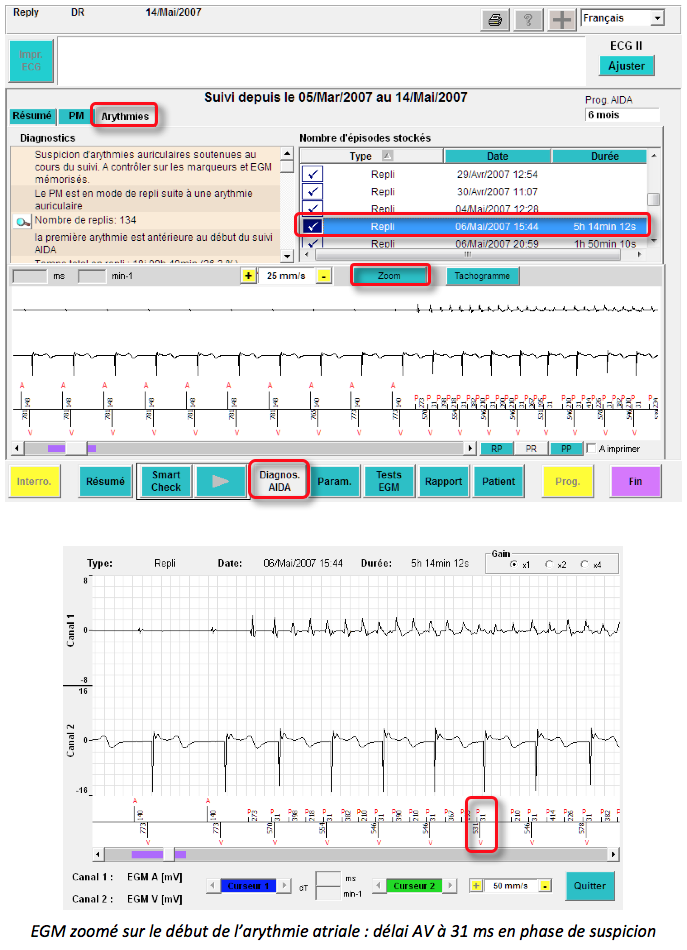
Phase of suspected atrial arrhythmia (N:1)
At the onset of rapid atrial rhythm, a short AV delay may be triggered on certain P wave detections in WARAD if and only if the R-V or V-V interval that would be applied is greater than 500 ms. This prevents overly rapid ventricular pacing at the start of the episode before switching to asynchronous mode. During this phase of suspected atrial rhythm disturbance, all detected atrial events are marked with refractory period markers (small “p”s). The WARAD value is then fixed at the WARAD value that detected the very first PAC and cannot exceed 500 ms. The short AV delay that can be triggered after certain P wave detections in WARAD is 30 ms (non-programmable).
Ventricular cycles with at least one atrial detection in the WARAD are considered “suspicious.”
How the mode-switch algorithm works
The fallback function consists of three distinct phases: a suspicion/confirmation phase, a dissociation phase, and a reassociation phase.
Suspicion/confirmation phase
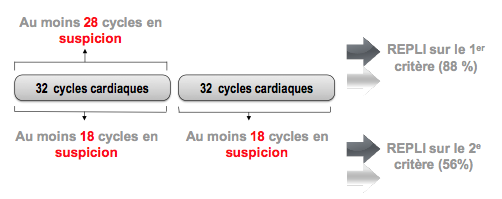
As soon as a ventricular cycle with suspected atrial arrhythmia is detected, the fallback algorithm begins an analysis of 32 ventricular cycles (repeated in blocks of 32 ventricular cycles if necessary).
Atrial arrhythmia is confirmed if one of the following two criteria is met:
- 28 or more ventricular cycles are suspected during the last 32 ventricular cycles (primary criterion)
- 18 or more ventricular cycles are suspected during the last two blocks of 32 ventricular cycles (secondary criterion)
The primary criterion is generally met in approximately 15 seconds. The secondary criterion may allow for a fallback despite atrial underdetection.
How the mode-switch algorithm works
The mode-switch function consists of three distinct phases: a suspicion/confirmation phase, a dissociation phase, and a reassociation phase.
Suspicion/confirmation phase
As soon as a ventricular cycle with suspected atrial arrhythmia is detected, the fallback algorithm begins an analysis of 32 ventricular cycles (repeated in blocks of 32 ventricular cycles if necessary).
Atrial arrhythmia is confirmed if one of the following two criteria is met:
- 28 or more ventricular cycles are suspected during the last 32 ventricular cycles (primary criterion)
- 18 or more ventricular cycles are suspected during the last two blocks of 32 ventricular cycles (secondary criterion)
The primary criterion is generally met in approximately 15 seconds. The secondary criterion may allow for a fallback despite atrial underdetection.
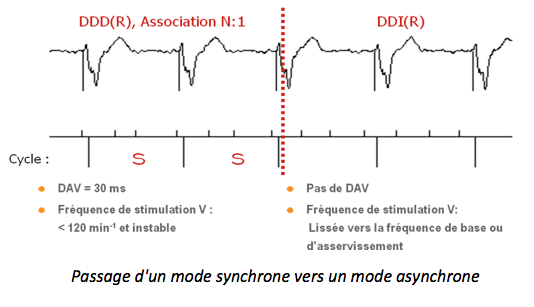
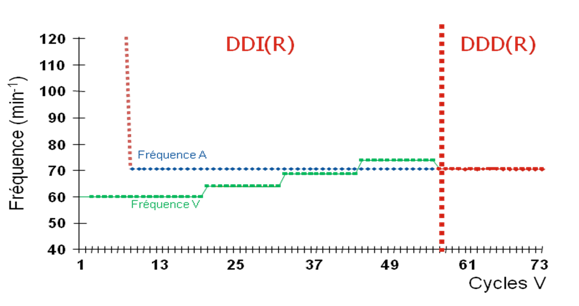
Dissociation phase
Once one of the retreat criteria is met, the pacing mode switches from a synchronous mode (DDD or AAI-SafeR) to an asynchronous mode (DDI). The ventricular pacing rate gradually decreases (the ventricular escape interval increases by 30 ms every 12 cycles) toward the base rate, the target rate, or the rest rate.
Reassociation phase
As soon as the atrial arrhythmia ceases and sinus rhythm resumes, the ventricular pacing rate is gradually adjusted to match the sinus rhythm. A-V reassociation only occurs if the atrial and ventricular rates are slower than 110 min-1. A 500 ms RetroPwatch is applied to the first reassociated ventricle to prevent the onset of a PMT.
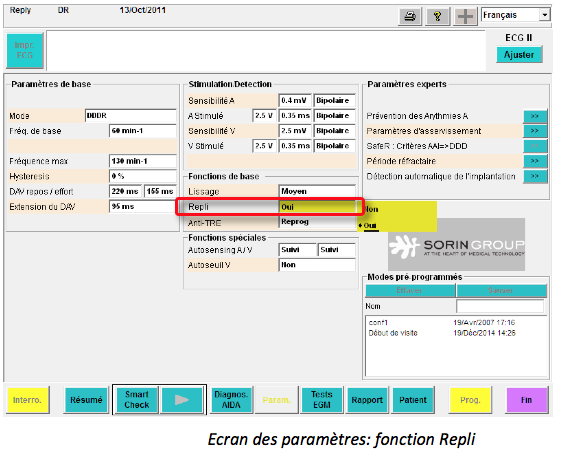
Mode-switch programming
The function is enabled by default.
Memory queries
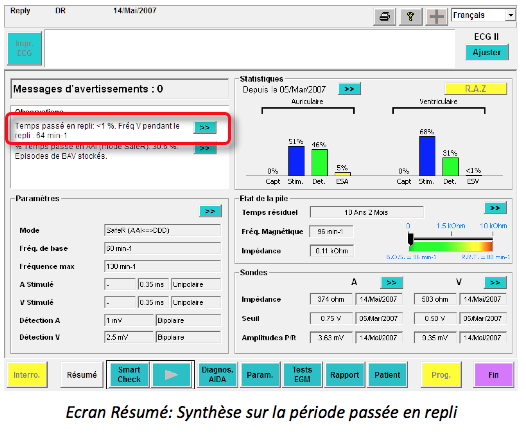
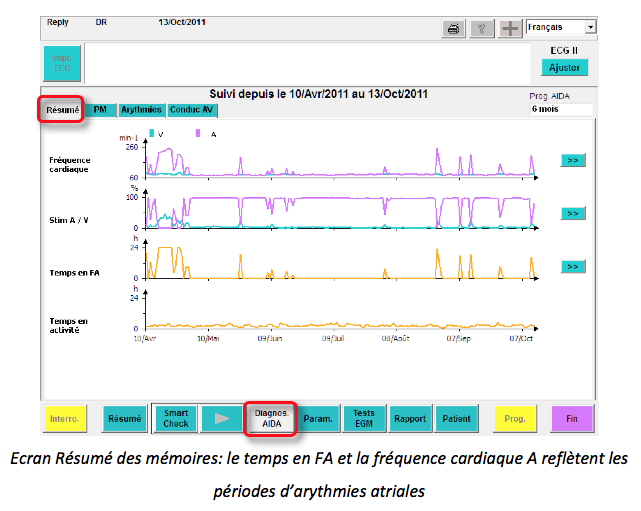
On the Summary screen, a comment is noted indicating:
- The time spent in withdrawal (in %)
- The ventricular frequency during withdrawal periods
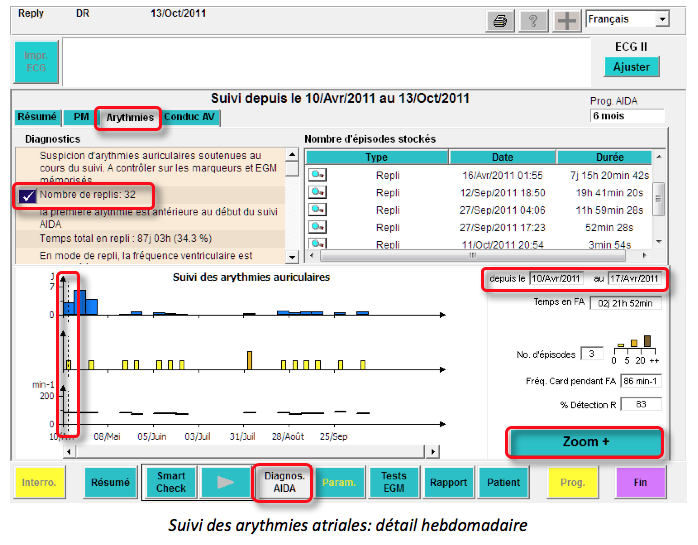
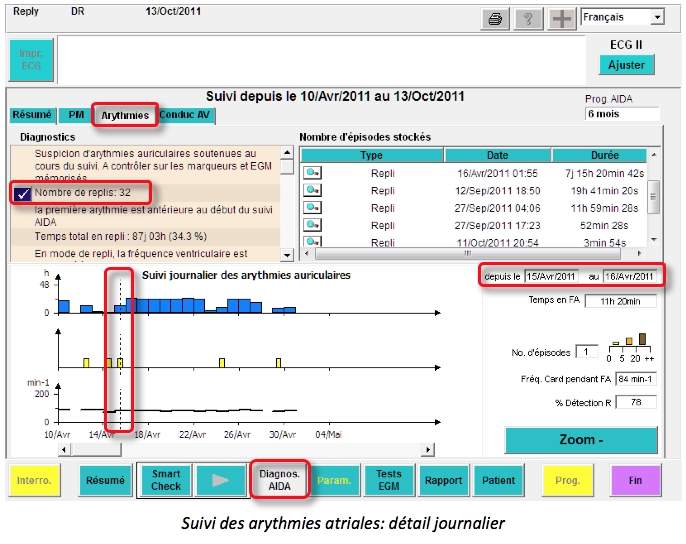
Another way to access the replay episodes is to click on Diagnos. AIDA and then on the Arrhythmia tab.
A detailed weekly or daily view shows: the duration of AF (time in retreat), the number of AF episodes, the ventricular rate, and the percentage of ventricular detections.
Flutter management
There is no algorithm of this type; when a 2/1 flutter occurs, it is necessary to shorten the duration of the atrial blanking period following ventricular pacing.
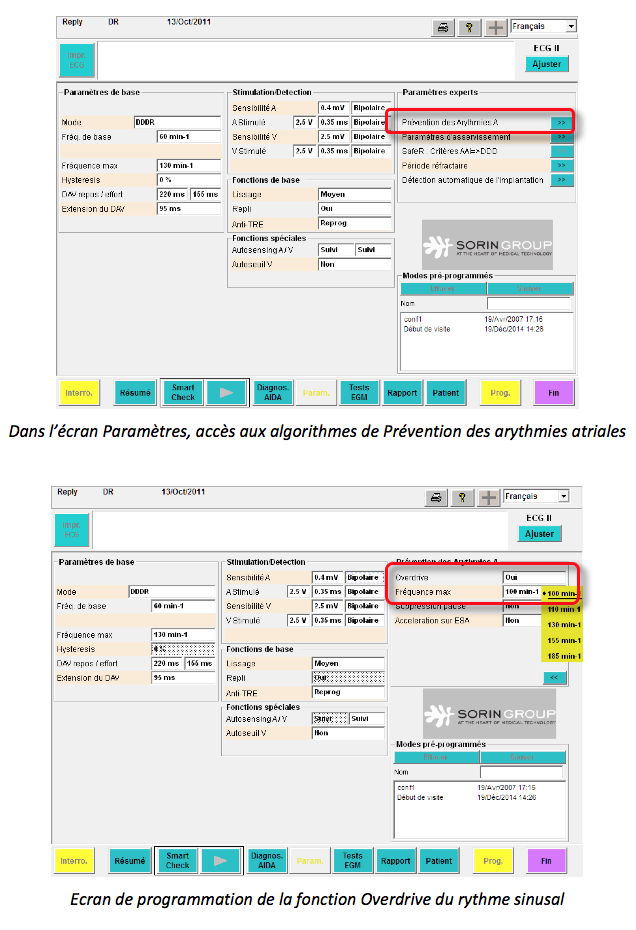
Atrial fibrillation prevention algorithm
Sinus rhythm overdrive
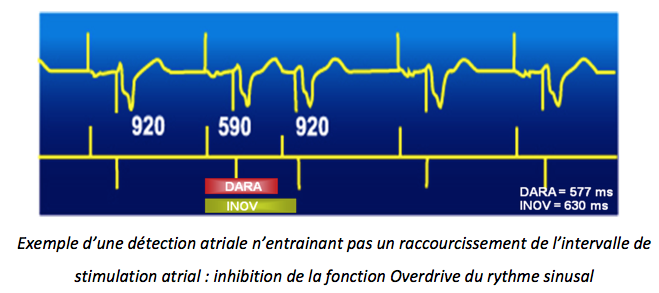
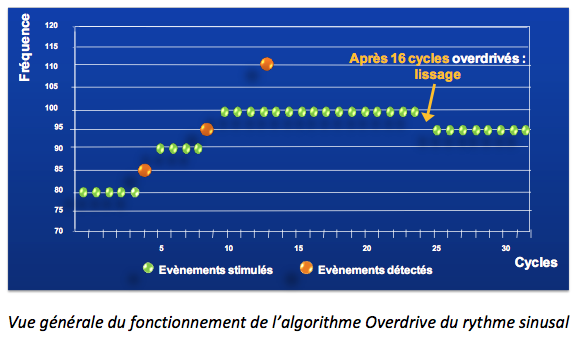
The objective is to ensure permanent atrial pacing slightly above sinus rhythm to prevent the onset of AF by reducing the atrial pacing interval (-50 ms) following the detection of non-accelerated P waves (detection outside the INOV window (and outside the DARA window)). This function is limited by a programmable maximum overdrive frequency. By default, this algorithm is inactive.
To avoid inappropriate acceleration on late atrial extrasystoles, there is a specific window (the INOV window, INappropriate OVerdriving). The value of this late ESA monitoring window is based on the AV or PR conduction time and the maximum overdrive frequency. If a P wave is detected in the INOV window, the sinus rhythm overdrive function is inhibited.
After 16 “overdriven” cycles, the stimulation frequency decreases with the programmed smoothing (very slow by default). The maximum overdrive frequency is programmed here at 100 min-1.
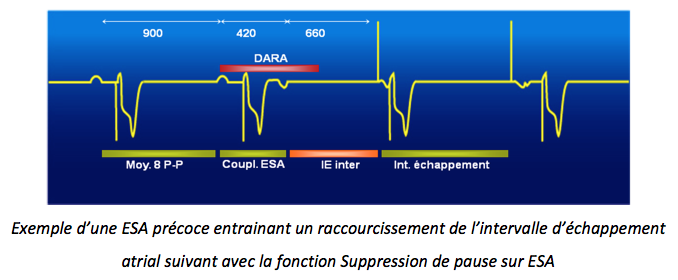
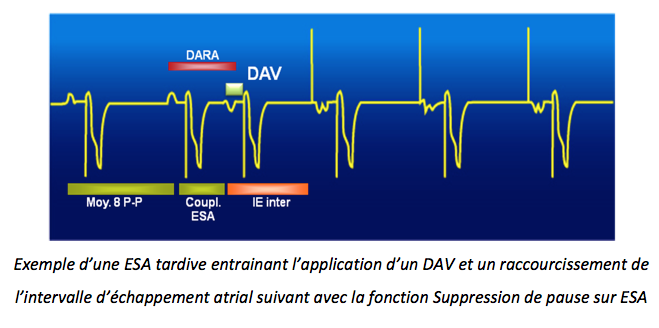
Elimination of pauses on PAC
The objective of this algorithm is to prevent the occurrence of atrial fibrillation on a succession of short atrial cycles (extrasystole) and long cycles (compensatory pause).
On an isolated “late” ESA (with coupling greater than 50% of the last P-P interval), the algorithm triggers an automatic AV delay and an intermediate escape interval.
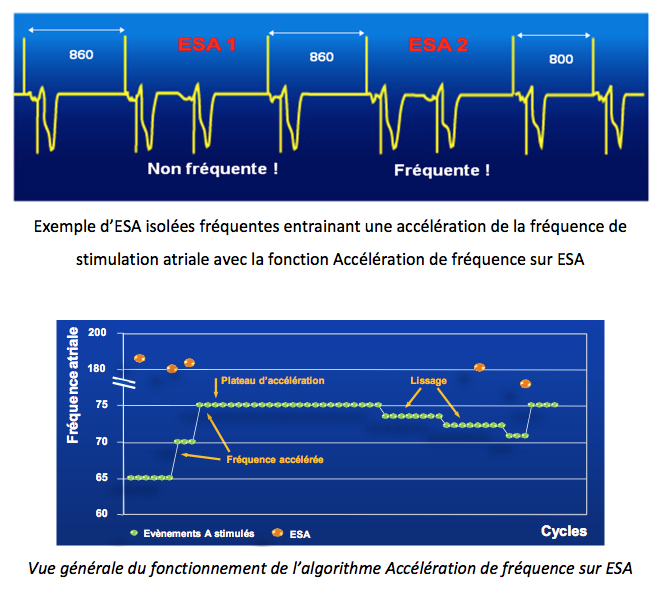
Frequency acceleration on PAC
To reduce the number of extrasystoles, this algorithm allows temporary frequency acceleration (~ 5 min-1) (24 cycles) following frequent isolated atrial extrasystoles (separated by a maximum of 15 normal atrial cycles). By default, this algorithm is inactive. The acceleration phase is stopped if the maximum acceleration rate is reached or if the maximum PAC counter is reached. These two stop criteria are not programmable. This stop is followed by a “definitive” smoothing to the base rate.
The maximum acceleration frequency is calculated as follows: if the atrial frequency is less than 90 min-1, the escape interval represents 75% of the average of the last eight P-P intervals just before the first PAC. Otherwise, the escape interval represents 75% of the average of the last eight P-P intervals just before the first PAC + 50 ms.