Short duration pacemaker-mediated tachycardia
Tracing
Manufacturer Medtronic
Device PM
N° 21
Patient
68-year-old man with ischemic cardiomyopathy, ejection fraction of 45%, on beta blocker therapy, implanted with an Adapta pacemaker for symptomatic paroxysmal sinus node dysfunction; the AV conduction is preserved with a normal PR interval; programming in DDD mode; consultation for palpitations and heart failure.
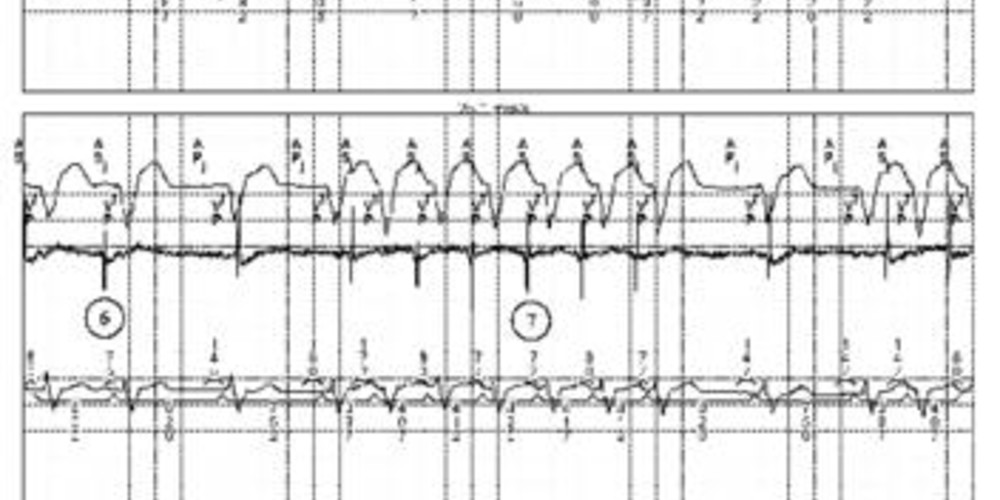
Graph and trace
The first line corresponds to lead I with the superimposed markers, the second line to the atrial EGM and the last line to lead II with the superimposed intervals;
- atrial sensing-ventricular pacing (AS-VP); the first question to ask is whether to program the DDD mode with ventricular pacing in this patient implanted for sinus dysfunction;
- slowing of the sinus rate and clearly ineffective AP pacing; the atrial EGM shows an activity occurring after the VP; this atrial activity is not sensed by the device since in the post-ventricular atrial blanking period; it is hence likely to be sinus activity and not retrograde conduction, the VP-atrial activity delay being too short; the pattern on the atrial EGM is substantially the same as that of the previous sinus AS;
- the sinus beat falls well behind the VP, is therefore labeled AS and leads to an AV delay and ventricular pacing;
- onset of a PMT with retrograde conduction; the pattern of the atrial EGM is now different from that observed on a sinus beat;
- the retrograde conduction remains fixed on 5 beats and then stops spontaneously causing the PMT to terminate; retrograde conduction is an indispensable element for PMT perpetuation;
- resumption of sinus rhythm (AS-VP);
- sequence identical to the previous sequence: sinus slowing, ineffective atrial pacing, PMT, spontaneous termination.
Other articles that may be of interest to you




This tracing is interesting since it depicts multiple PMT episodes which terminate spontaneously. The PMT interruption algorithm is programmed, however the episodes are too short and consequently the algorithm does not intervene (at least 8 consecutive intervals are needed for the diagnostic algorithm to interrupt a PMT). These repetitive tachycardia episodes are probably responsible for cardiac decompensation. In this patient, it seems necessary to: