Blanking, safety window, atrioventricular delay
Tracing
Manufacturer Medtronic
Device PM
N° 18
Patient
61-year-old man implanted with a dual-chamber pacemaker for syncopal paroxysmal sinoatrial block; programming in DDD mode; routine consultation and recording of the tracing.
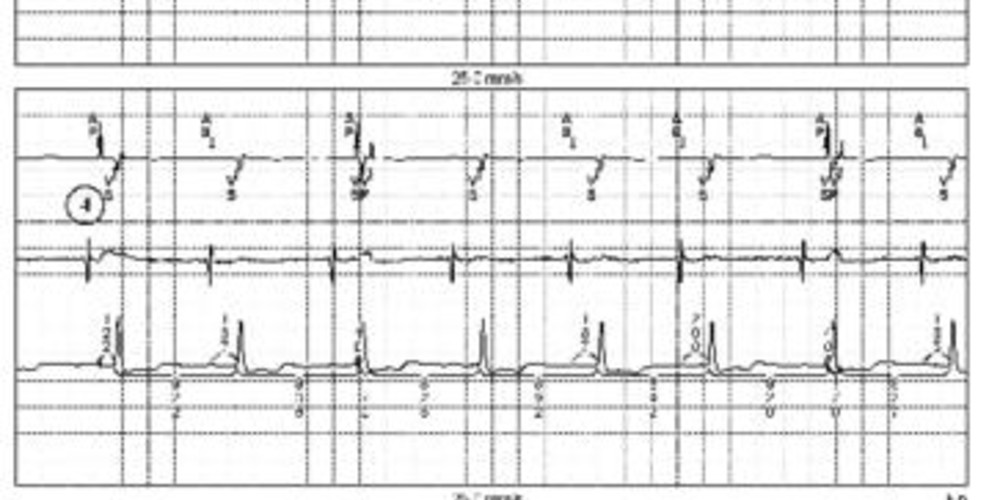
Graph and trace
The first line corresponds to lead III on which the markers are superimposed, the second line to the atrial EGM and the third line to lead II with the intervals;
- AS-VS interval properly detected;
- atrial undersensing; the atrial EGM shows an atrial signal not sensed by the pacemaker; in the absence of atrial sensing, atrial pacing (AP) at the end of the escape interval; the spontaneous QRS conducted from the AS that was not detected falls immediately behind the AP in the post-atrial ventricular blanking period; this spontaneous ventricular event is therefore not sensed and does not interrupt the AV delay; ventricular pacing occurring at the end of the AV delay is not effective; this pacing is hazardous since it falls on the T wave of the previous spontaneous ventricular complex;
- identical sequence (atrial undersensing, atrial pacing and spontaneous ventricle); the spontaneous ventricle is no longer in the blanking period but in the safety window; it is thus sensed and generates a pacing at the end of the safety window which is not effective and not dangerous because in the absolute refractory period of the preceding spontaneous ventricle;
- identical sequence (atrial undersensing, atrial pacing and spontaneous ventricle); the spontaneous ventricle is no longer in the blanking period nor in the safety window but in the end of the AV delay; it therefore inhibits ventricular pacing.
Other articles that may be of interest to you





This tracing corresponds to a problem of intermittent atrial undersensing. The remainder of the functioning is strictly normal. This tracing allows detailing the 3 ventricular periods following an atrial pacing, namely blanking, safety window and end of AV delay, and shows the behavior of the pacemaker during sensing in each of these periods. There is no ventricular blanking or safety window after the sensing of an atrial signal.
Post-atrial ventricular blanking is intended to avoid sensing of the atrial stimulus by the ventricular sensing chain which would result in ventricular inhibition. A ventricular signal occurring during post-atrial ventricular blanking is not detected; it does not inhibit ventricular pacing at the end of the programmed AV delay. If this blanking is programmed too short, the risk of sensing the atrial stimulus in the safety window is high, resulting in permanently forced ventricular pacing with a short AV delay of 110 ms. This too short AV delay may have hemodynamic deleterious effects. If the blanking is programmed too long, this can be problematic if a late PVC occurs. There is indeed a significant risk of pacing in the vulnerable period at the end of the AV delay (a PVC in the blanking does not modify the behavior of the pacemaker which paces at the end of the programmed AV delay). This risk is all the more substantial when the blanking and AV delay are programmed long.
The safety window is a ventricular sensing period complementary to post-atrial ventricular blanking. It is initiated only after atrial pacing and is designed to prevent ventricular asystole due to inappropriate inhibition of ventricular pacing by late sensing of the stimulus or of atrial depolarization. The duration of the safety window is not programmable and is fixed at 110 ms. Ventricular sensing within 110 ms after atrial pacing is considered non-physiological and causes ventricular pacing at 110 ms or at the end of the paced AV delay, if the latter is less than 110 ms. The 2 VP and VS annotations appear on the real-time rhythm monitor, on the « frozen » tracings and on the printed tracings.
The short AV-delay pattern allows identifying pacing in the safety window on the electrocardiogram. If the event sensed in the safety window is the result of crosstalk or oversensing of noise, the pacing pulse allows a 110 ms ventricular capture after the atrial stimulus. If the event sensed in the safety window corresponds to a late PVC or atrioventricular conduction, the pacing at the end of the safety window occurs sufficiently early in the absolute myocardial ventricular refractory period to avoid pacing at the peak of the T wave. Ventricular safety pacing can be programmed to ON or OFF, but is preferentially programmed ON, particularly in pacemaker-dependent patients.
In this patient, the troublesome issue is that of an intermittent atrial undersensing. Adaptation of atrial sensing allowed resolving the problem.