Shock in the VT zone
Tracing
Manufacturer Medtronic
Device ICD
Field Therapy
N° 17
Patient
Patient implanted with dual-chamber ICD (Entrust DR) for ischemic cardiomyopathy; consultation for electrical shock.
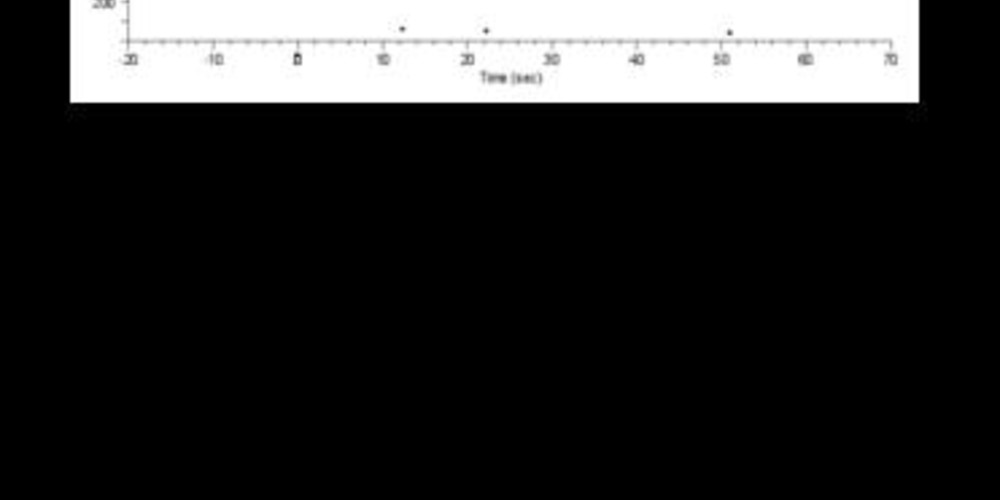
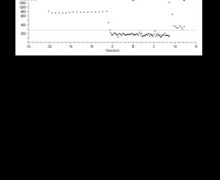
Graph and trace
The graph shows a probable ventricular arrhythmia detected in the VT zone, treated successively with 6 sequences of anti-tachycardia pacing (3 bursts followed by 3 ramps) which do not allow the return to sinus rhythm followed by an electrical shock of 10 Joules with successful termination.
- the EGM confirms ventricular tachycardia with atrioventricular dissociation;
- 3 successive bursts (fixed rate) which prove ineffective;
- 3 ramps (increment between each stimulus);
- the ensuing therapy is an electrical shock;
- after a very short charge time, an electrical shock of 10 Joules is delivered;
- successful shock and termination of the arrhythmia.
Other articles that may be of interest to you




In the absence of an optimal universal programming, the results of large-scale studies concur on the need to limit the incidence of inappropriate or unnecessary therapies without jeopardizing patient safety and to prioritize anti-tachycardia pacing in lieu of electrical shocks. It is customary to program increasingly aggressive therapies and anti-tachycardia pacing represents the first-line treatment for monomorphic tachycardia. In the VT zone (<200 beats/minute), a series of bursts rather than ramps (Class I indication) is therefore usually programmed. Indeed, the ratio between termination and acceleration of the arrhythmia appears to favor burst therapy (identical efficacy but less prominent pro-arrhythmogenic feature) compared to the ramp. If the bursts prove unsuccessful, it is then possible to program a series of ramps to promote a painless therapy and subsequently a series of electrical shocks. In this example, a shock of 10 Joules allows terminating the arrhythmia and the return to sinus rhythm. Various parameters influence the choice of the amplitude of the first shock in the VT zone, which can be programmed at maximum energy or at a lower amplitude (in the order of 10 Joules). A certain number of advantages can be found in programming a first shock of moderate amplitude (10 Joules):