Single chamber discrimination: atrial tachycardia
This 54-year-old man, recipient of a Abbott Atlas single chamber ICD implanted in the context of hypertrophic cardiomyopathy with a 32-mm thick septum, episodes of non-sustained VT and failure to adapt the blood pressure during exercise, was seen for a routine follow-up visit.
Main programmed parameters
- VF zone at 207 bpm and VT zone at 160 bpm
- 12 cycles in the VF zone and 20 cycles in the VT zone were needed for the diagnosis
- Effective discrimination programmed in the VT zone
- Number of criteria for a VT diagnosis: 2 out of 3
- Morphology: ON (60%; 5 out of 8)
- Stability: ON 40 ms; detection window: 12 intervals
- SIH: passive, 2 intervals
- Sudden onset: ON, 20%
Narrative
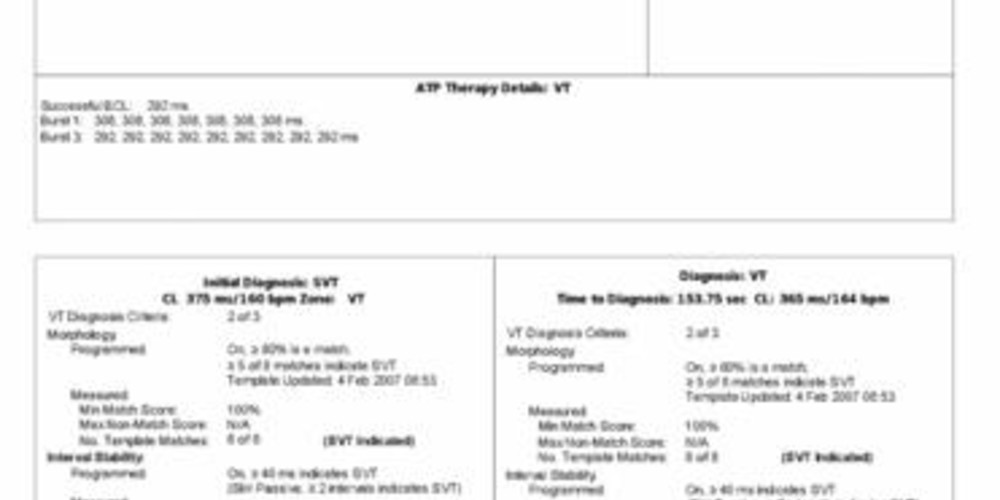
Episode initially diagnosed as SVT; 2 out of 3 discrimination criteria were needed for the diagnosis of VT. The morphology and sudden onset criteria were in favor of SVT and the stability criterion in favor of VT. The SIH counter, in favor of SVT, was not included in the analysis since it was set on “passive”. Consequently, no therapy was delivered.
After SVT was diagnosed, the analysis continued until the possible return to sinus rhythm. When the sudden onset criterion switched in favor of VT, 2 out of 3 criteria now favored VT, triggering 3 bursts of ATP, following the delivery of which the heart rate, although still rapid, was below the VT rate.
Tracing
- rapid and regular rhythm in the sinus zone (VS) with morphology flawlessly similar to the reference. After 5 consecutive VS, return to sinus rhythm was diagnosed;
- first cycle of the episode classified in the tachycardia or fibrillation zone (in this case T); the gradual versus sudden onset of the tachyarrhythmia was ascertained from this pivotal cycle onward; the variations in heart rate preceding this cycle are subtle, explaining the failure of the device to sense a sudden onset; it is also from this cycle onward that the number of sinus and unclassified intervals included in the SIH counter were counted;
- from this complex onward, 12 cycles elapsed before the diagnosis; stability was analyzed during these 12 cycles;
- from this complex onward, 8 cycles elapsed before the diagnosis; morphology was analyzed during these 8 cycles;
- once the VT counter was full, the diagnosis was made (12 cycles classified T since the previous return to sinus rhythm); the 8 ventricular electrograms analyzed by the morphology criterion were considered similar (100, ν), as the percentage of similarity was consistently above the programmed 60% threshold. Out of the 12 analyzed cycles, the second shortest and the second longest were measured at, respectively, 367 and 383 ms, representing a 16 ms delta (rounded up to 15 ms). This criterion favored VT; on the other hand, starting with the first T cycle, 6 VS + 10 unclassified intervals elapsed: the SIH counter = 16 favored SVT; however, since it was “passive”, it was not included in the analysis. Two criteria (gradual onset + similar morphology) being in favor of SVT, no therapy was delivered;
- redetection after 6 cycles classified as T; in absence of sudden onset and presence of similar morphology, the diagnosis was SVT; a new analysis during the episode classified all 6 cycles as T;
- ventricular undersensing probably due to ventricular extrasystole, causing a spuriously long cycle lasting 723 ms;
- if the sudden onset criterion is initially in favor of SVT (gradual onset), it is systematically recalculated during subsequent redetections; the spuriously long cycle activated the sudden onset criterion (measured here at 20%, which was the programmed limit for its activation); it was included in the average of 4 out of 8 preceding cycles (taking alternatively 1 out of 2 intervals); since 2 criteria (sudden onset + stability) were in favor of VT à VT was diagnosed;
- burst of 8 stimuli;
- redetection after the burst; in this phase of redetection, morphology is no longer analyzed;
- second burst following 6 cycles classified T;
- another redetection;
- third burst following 6 cycles classified T;
- subtle slowing of the heart rate; diagnosis of return to sinus rhythm after 5 VS without intervening T cycle.





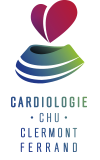
This tracing highlights the challenges represented by the discrimination of atrial tachycardia or atrial flutter, in which 2 criteria out of 3 typically indicate VT. The onset may be sudden (VT), the rhythm is stable (VT) and the morphology is similar (SVT). Therefore, the recommended programming of 2 out of 3 parameters does not guarantee effective discrimination. In patients presenting with this arrhythmia history, the programming of 3 out of 3 parameters (all indicating the presence of VT) is advised.
This tracing, however, has its specific nuances:
1) the onset was sensed as gradual, as the rate of the tachycardia hovered around the lower limit of the VT zone, without sudden change in rate when the tachycardia entered the VT zone. This episode of atrial tachycardia was initially diagnosed accurately, a relatively rare occurrence when 2 out of 3 parameters are programmed;
2) the 3 parameters were continuously analyzed throughout the episode. An undersensed ventricular extrasystole caused a pseudo-prolonged diastole, which activated the sudden onset criterion, as the programmed 20% threshold value was reached. The device diagnosed an episode of VT and delivered 3 salvos of inappropriate ATP.