Tachycardia treated with a shock, or is it?
Patient
A 70-year old patient is implanted with a dual lead ICD (ULYS DF4) in the context of secondary prevention (VF) in ischemic cardiomyopathy.
You interrogate the device in the emergency department after sensation of lightheadedness:



Interpretation
This case shows an episode of very fast polymorphic ventricular arrhythmia, which self terminates before the delivery of a shock.
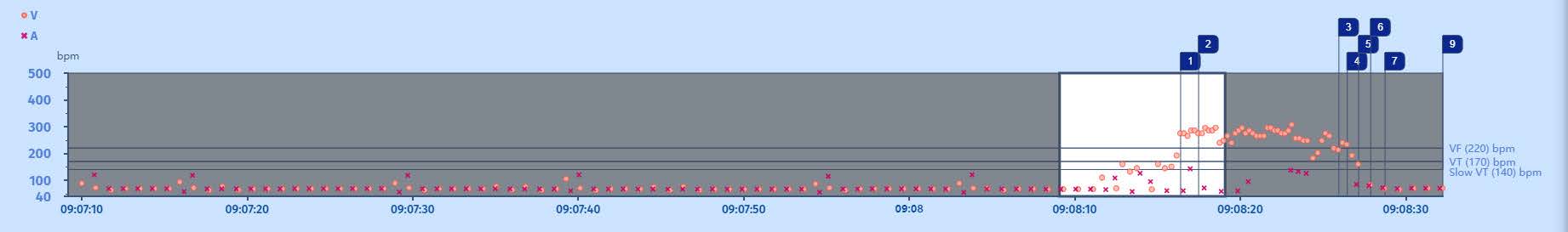
Interval plot
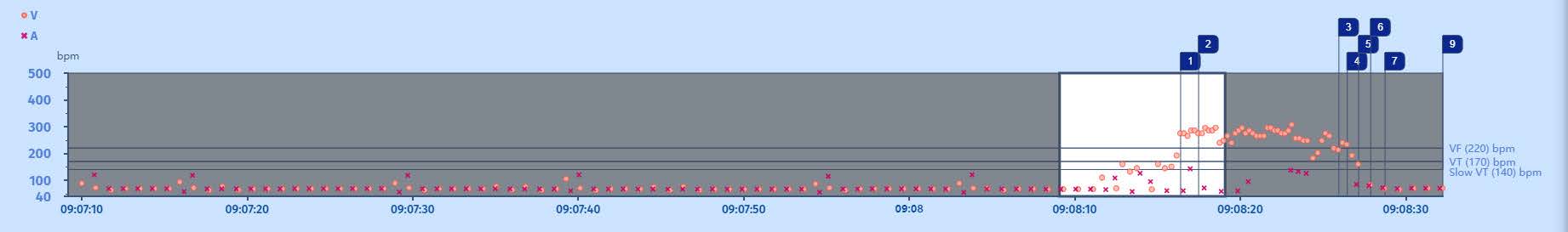
The interval plot shows a stable and slow rhythm (probably paced) with some extrasystoles when suddenly there is a ventricular arrhythmia in the VF zone (>220/min). As the ventricular arrhythmia accelerates into the VF zone. After a while the arrhythmia slows down, becomes more irregular and self-terminates.
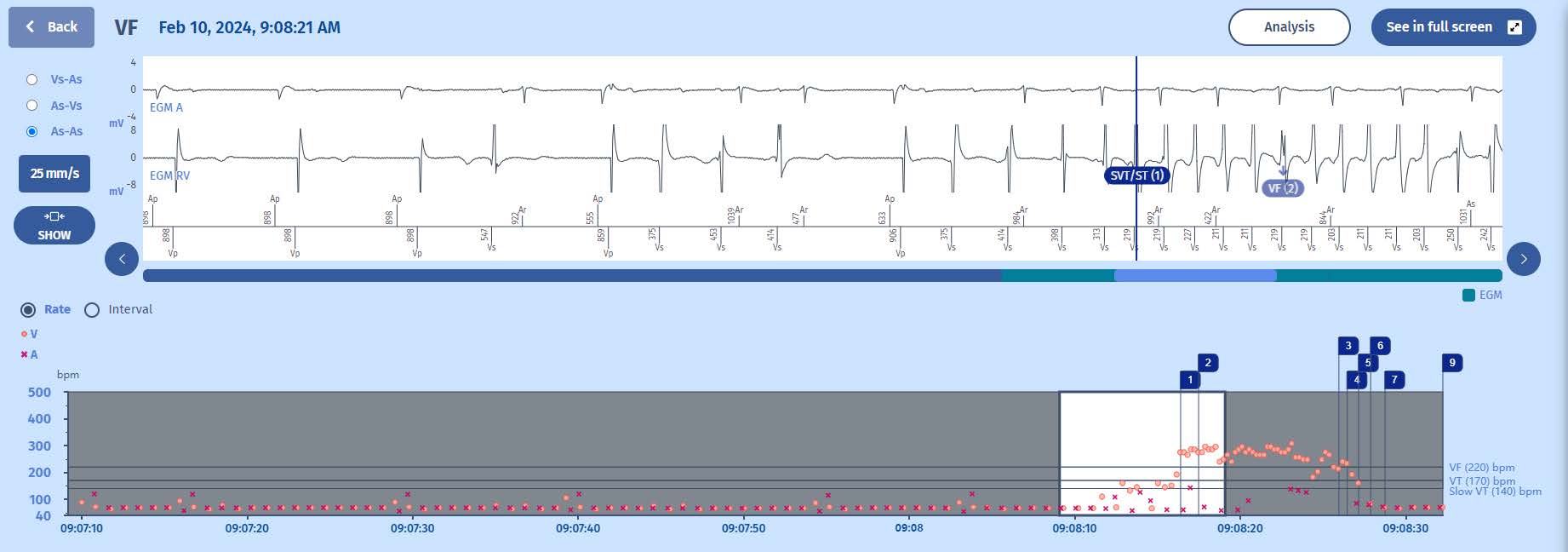
EGM
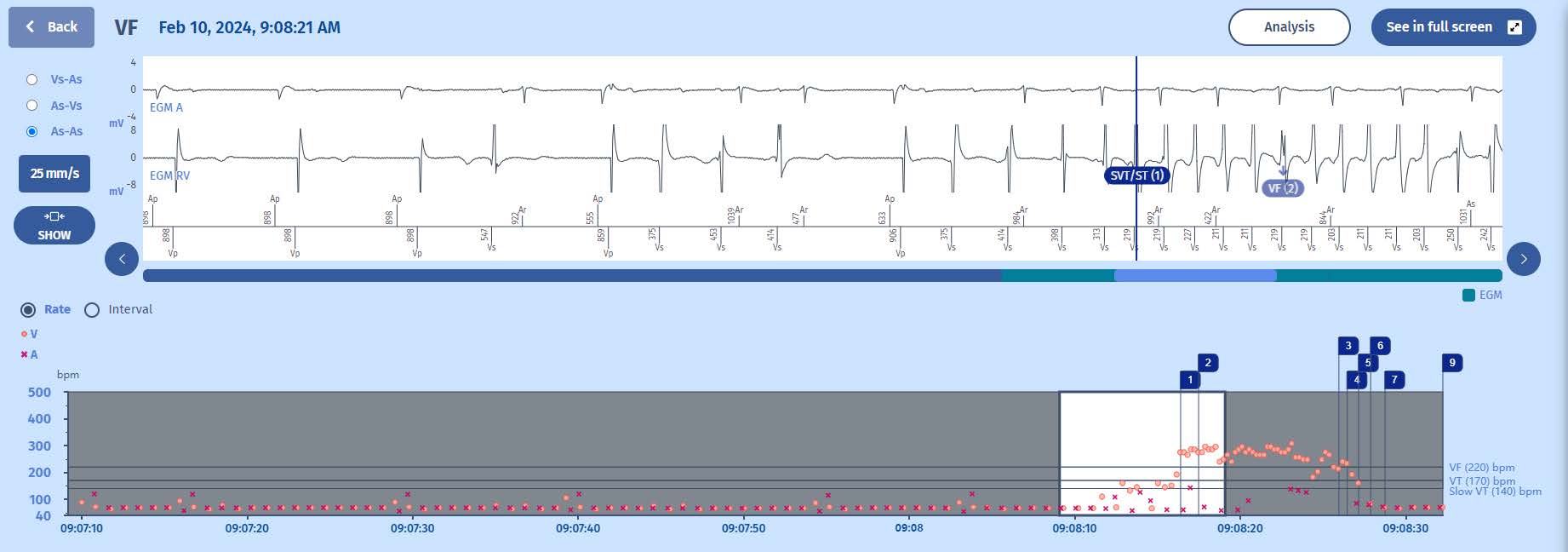
The VT majority is first filled but as it is irregular, it is classified as SVT by the PARAD discrimination algorithm. Soon after, the VF counter is filled with 6 ventricular events in the VF zone and the persistence counter starts.
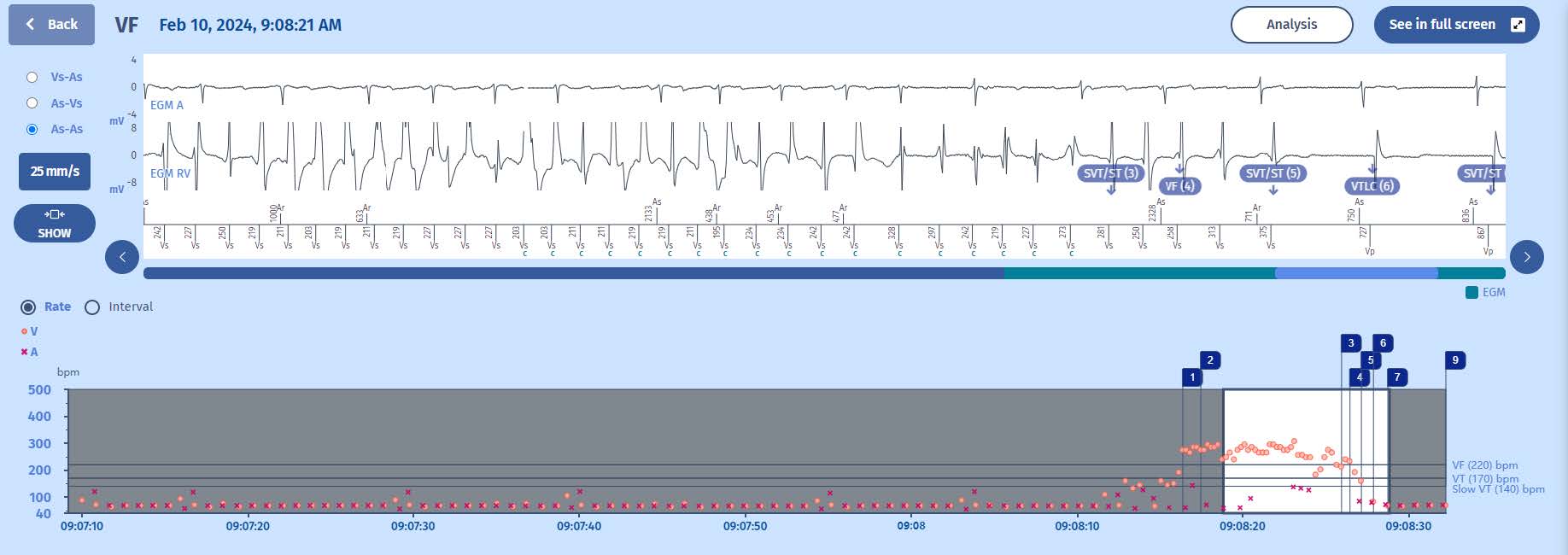
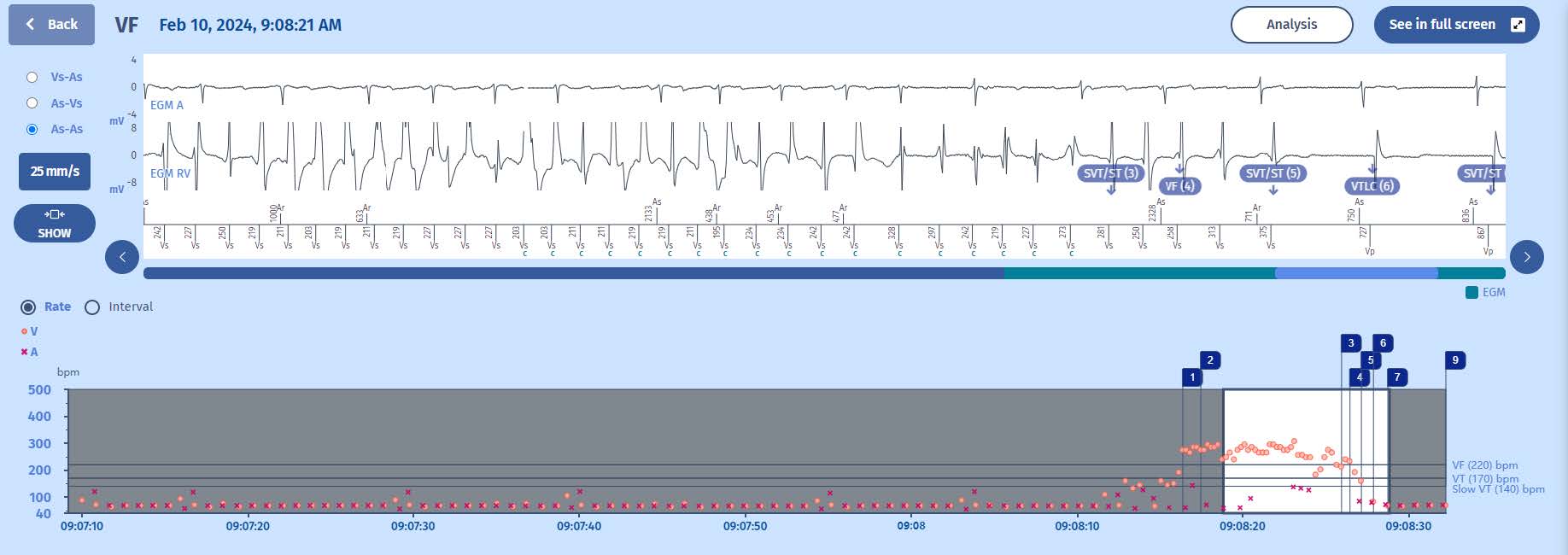
When the persistence counter is filled (20) and as the arrhythmia is too irregular to deliver ATP (Fast VT therapy), the ICD starts to charge in order to deliver a shock. In order for the ICD to continue charging, the VF majority must be met. As soon as we see the
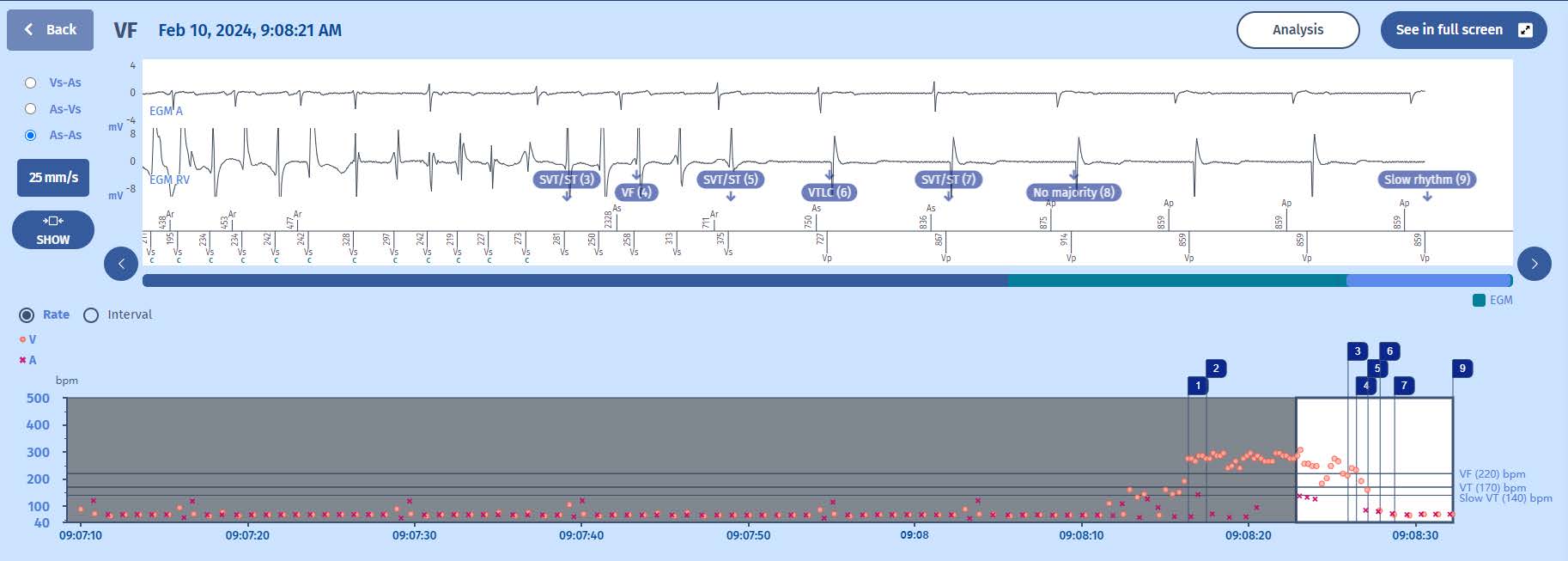
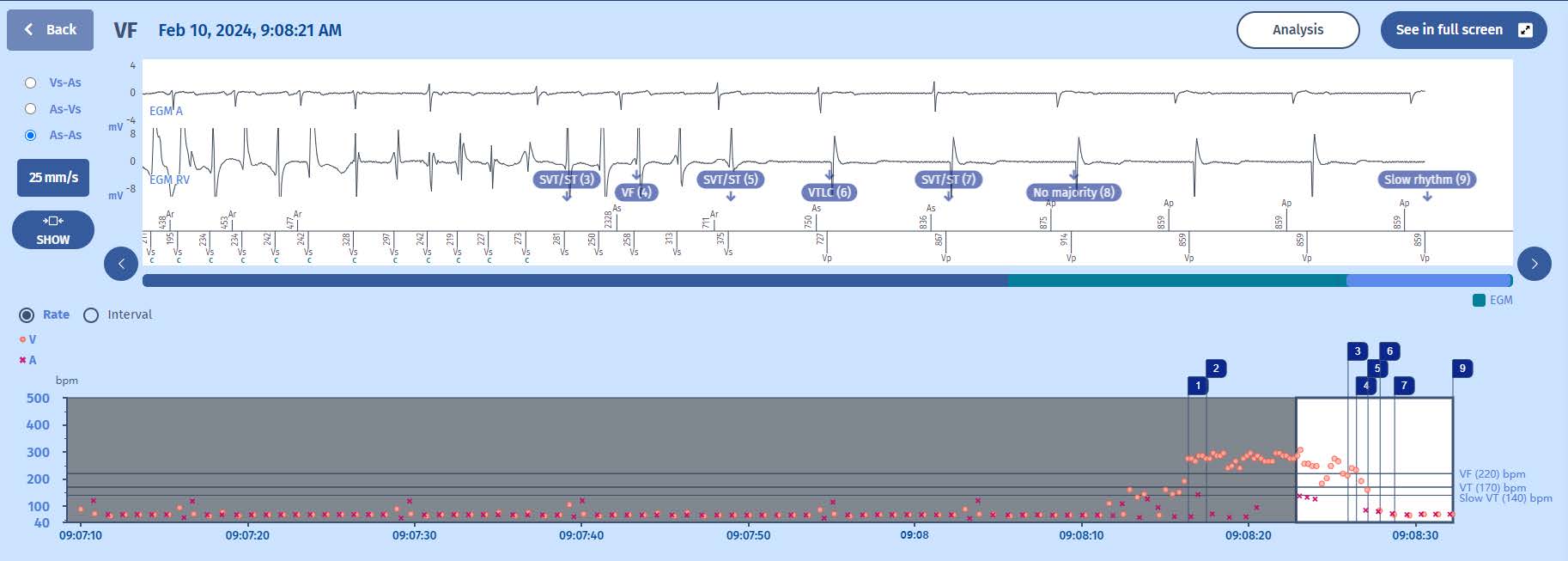
SVT marker, the ICD stops charging as the VF majority is lost. On the EGM we can confirm that the ventricular arrhythmia slows down into the VT zone but also becomes irregular (which is why we see a SVT marker). Soon after we see multiple markers as the arrhythmia is flirting with the VT (but unstable therefore SVT) and VF zones. Note also that while we see a new VF marker, there is no continuation of the charge (no blue c). This is because while the VF counter is filled, the persistence counter is not and therefore the charge remains aborted. Soon after, the arrhythmia self terminates and no shock is delivered.
Comments
While at the dawn of ICD therapy, we were most worried about correctly sensing the episode and delivering the shock as fast as possible, the dogma has completely changed. Today, we demand of our contemporary ICDs not only to correctly detect episodes and deliver fast and efficient therapies, we also demand a near-zero rate of unneeded or inappropriate therapies. Therefore, the counters must seamlessly work together with the other existing algorithms and past mistakes make for good learning. Today, we see that counters are getting longer and longer, mostly with the goal to decrease therapies which are not needed or not appropriate. In this case, we see a good example of an aborted charge for good reasons; the self-termination of the ventricular arrhythmia. We now understand why for the charge to continue, the majority and persistence of VF (or VT when in VT zone) must be met. When the patient will again suffer for a ventricular arrhythmia soon after, the charge will be faster as the consensators will not actively dump the
charge. This is why we can see surprisingly fast charge times during some episodes.
A full charge of an ICD can consume multiple weeks of battery capacity and therefore major efforts must be taken to prevent charges and shocks which are not needed or inappropriate.
This is why the VT/VF majority and persistence must be met for each cycle for the charge to continue.