T-wave oversensing
Patient
54 year old patients with dilated cardiomyopathy and left bundle branch block, implanted with a CRT-D, comes in for a regular device check-up.

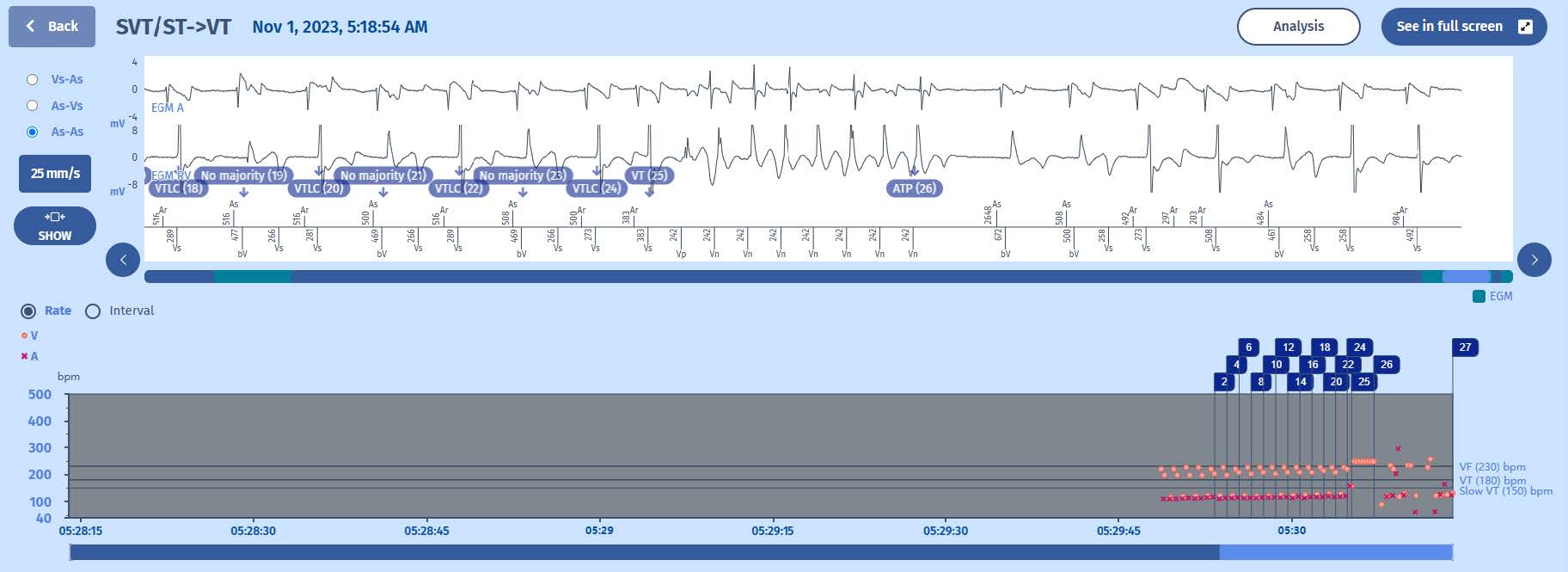
EGM

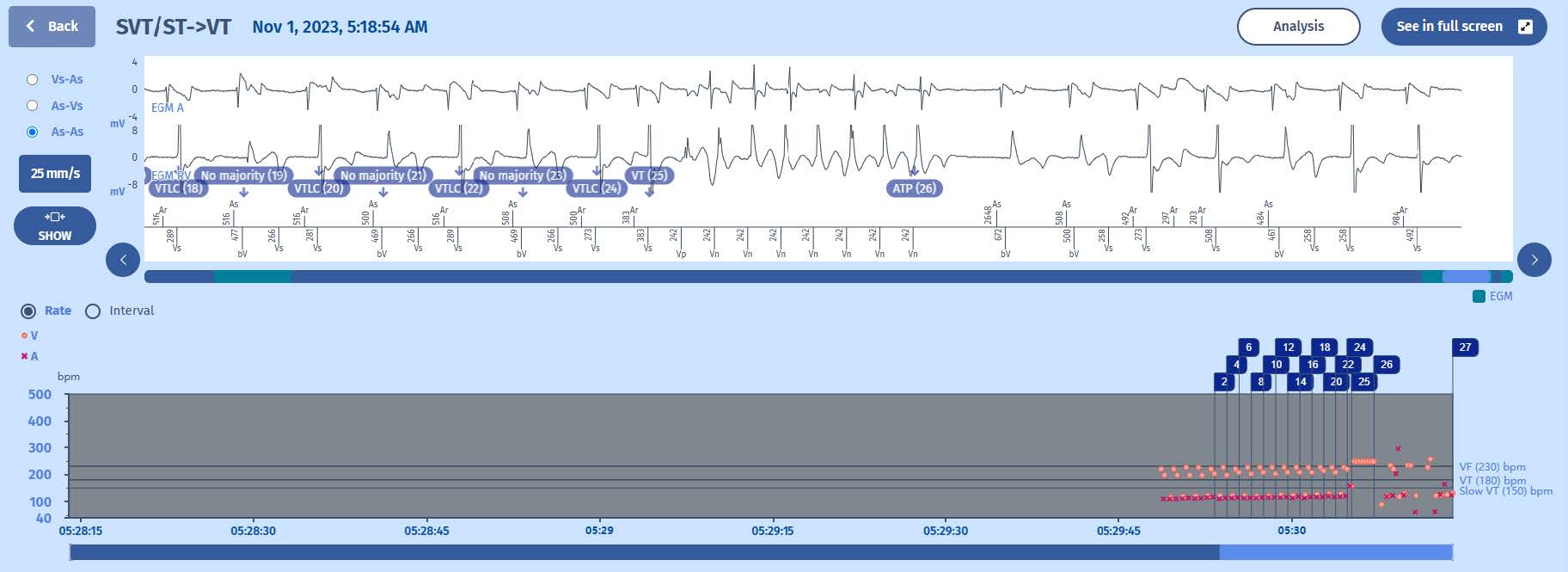
Rate interval plot
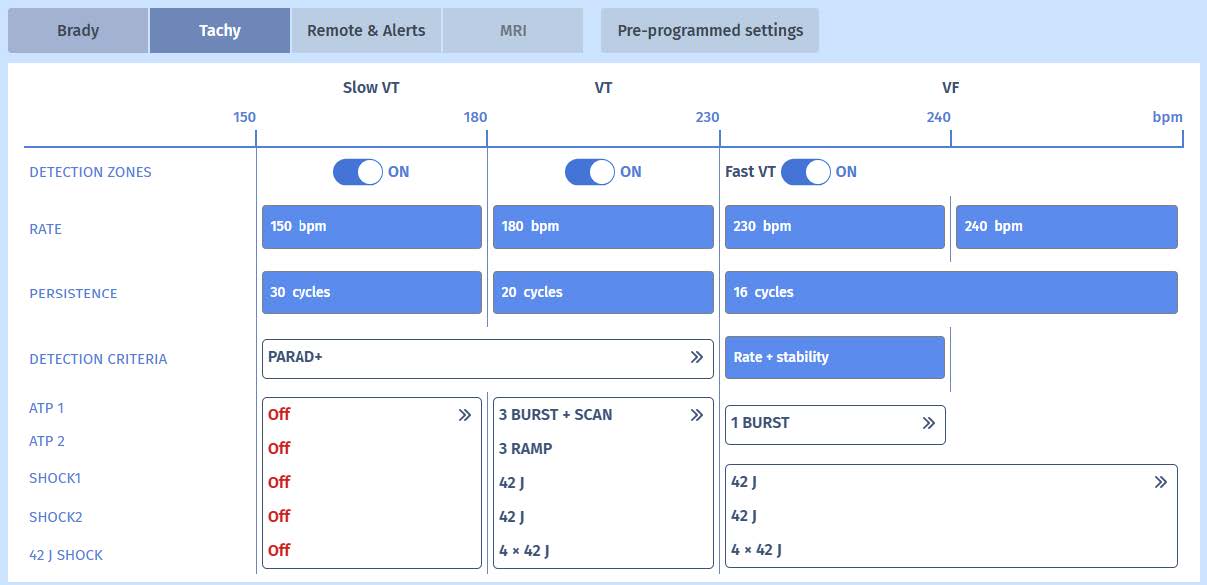
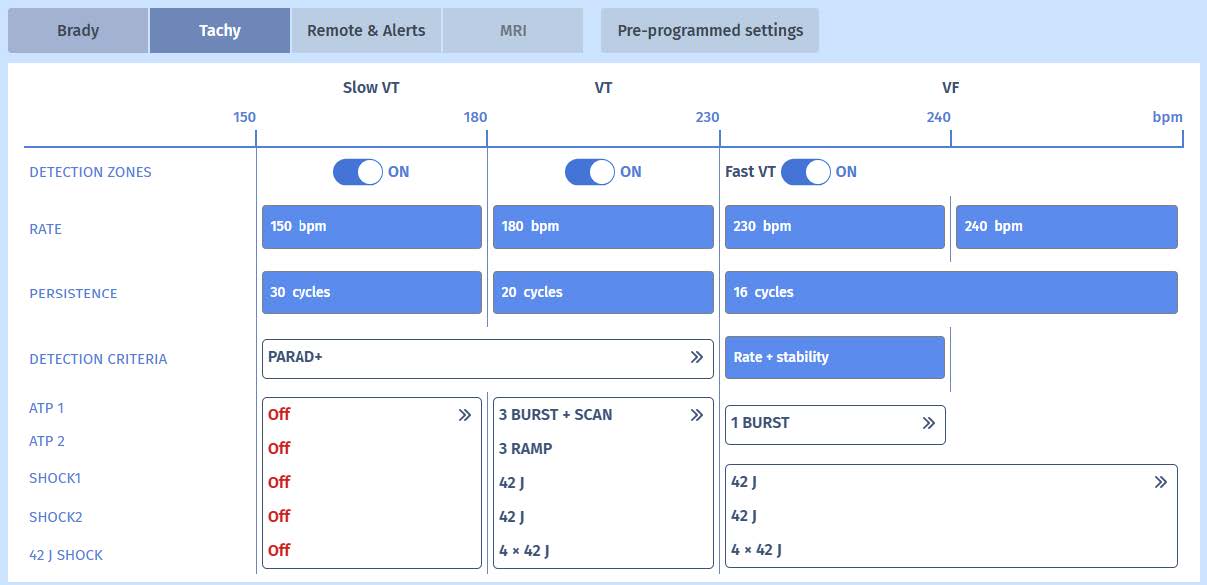
A typical feature of T-wave oversensing is that it creates a typical pattern with very short cycles (R-to-T) and short cycles (T-to-R). This creates a typical “railtrack track” pattern on the rate interval plot which is associated with oversensing of physiological signals (P-wave, R-wave or such as in this case T-wave oversensing). The pattern will suddenly appear and disappear and has only very slight variations in rate while the underlying rhythm is often sinus tachycardia (in order for the
short cycles to be short enough to cross the VT zone).
EGM
The baseline rhythm is atrial sensing (sinus tachycardia) and biventricular pacing. Throughout the episode, we see a certain pattern. It begins with oversensed T-waves after biventricular pacing. These short cycles disable the delivery of biventricular pacing after the following atrial cycle and we see intrinsic atrioventricular conduction. The cycle thereafter does again allow biventricular tracking and we again see T-wave oversensing. This pattern repeats itself during acceleration of sinus rhythm which also makes the cycle after T-wave oversensing fast enough to fill the VT counter. Interestingly, the rhythm is considered stable as the majority (6/8) is indeed stable. We see many VTLC markers without therapy because the slow cycles change the diagnosis to “No
majority” and they also extend the persistence (part of the PARAD+ algorithm). As there are no “SVT/ST” or “Slow rhythm” majorities, the persistence is never reset. Suddenly, because of the appearance of a premature atrial complex (PAC), the PARAD+ find AV association and follows a different path (VTLC -> VT). The slow cycles no longer extend the persistence which is filled (never set to 0 by SVT or slow rhythm markers) and an ATP is delivered.
Comments
T-wave oversensing is extremely rare in MicroPort devices even though it is still a common phenomenon across other ICD platforms. The engineers have succeeded in filtering out the T-waves so that they are rarely oversensed these days. While it is true that in most cases of T-wave oversensing (across all ICD platforms), there is an association with small amplitude R-waves and increased risk of T-wave oversensing due to the adaptive sensitivity in ICDs (more sensitive during the cycle after small R-waves), However, this is not the case in the current patient as the R-waves are of significant amplitude (>15 mV). In addition, the oversensed T-waves are only to be found after biventricular paced events, which is very uncommon for tachycardia episodes. Pacing may
indeed alter the morphology and amplitude of T-waves but rarely causes inappropriate therapies because of the low rate at which pacing occurs, limited also by the higher upper tracking rate. For a MicroPort ICD to deliver inappropriate therapy (a single ATP burst in this case), we must reach 6 out of 8 cycles in the VT zone. During biventricular pacing with T-wave oversensing, we only expect 4 out of 8 cycles to be within the VT zone as the R-T interval is very short (260-270 ms in this case)
and the T-R interval is not. This is one of the main reasons why majority is set at 75% (6 out of 8) for the VT and VF counters, it protects the patient against inappropriate therapy due to T-wave oversensing. However, when the patient’s sinus rhythm accelerates beyond a certain heart rate, the T-R intervals shorten and may cross the VT zone. We can see that the patient’s heart rate is indeed >110/min and the VT counter is filled. Slow cycles prolong the onset of therapy because their presence leads to a classification of the rhythm as ‘No Majority’, which does not influence the VT persistence counter.In this patient, there is a single episode of T-wave oversensing among many episodes of true ventricular arrhythmia. There were no programming changes made.125
Solutions for T-wave oversensing are not abundant. Changing the sensitivity is often the first thought but it may also impair the ability of the ICD to adequately detect VF signals, especially when the R-wave amplitude is low. Changing the zones will most often not help as the VT/VF counters are filled at high rate (including in this case). The true danger of T-wave oversensing is that it may deliver a shock on the T-wave (the ICD considering it to be a fast ventricular event on which it should deliver the shock), with potential catastrophic results (inducing a true VF which may be hard to defibrillate). In some companies with higher risk of T-wave oversensing there are other programming changes to be considered (changing the sensing vector, changing the adaptive
sensing parameters) but in some cases, a new RV lead needs to be placed to solve the issue.
Take home message
T-wave oversensing is extremely rare in MicroPort devices but needs to be timely recognized and managed even though programming options are mostly limited.