Possible deleterious effect of antitachycardia pacing
Patient
A 56-year-old ischemic patient, with ejection fraction of 30% and symptoms of heart failure, implanted with a dual chamber defibrillator, comes for a routine check.
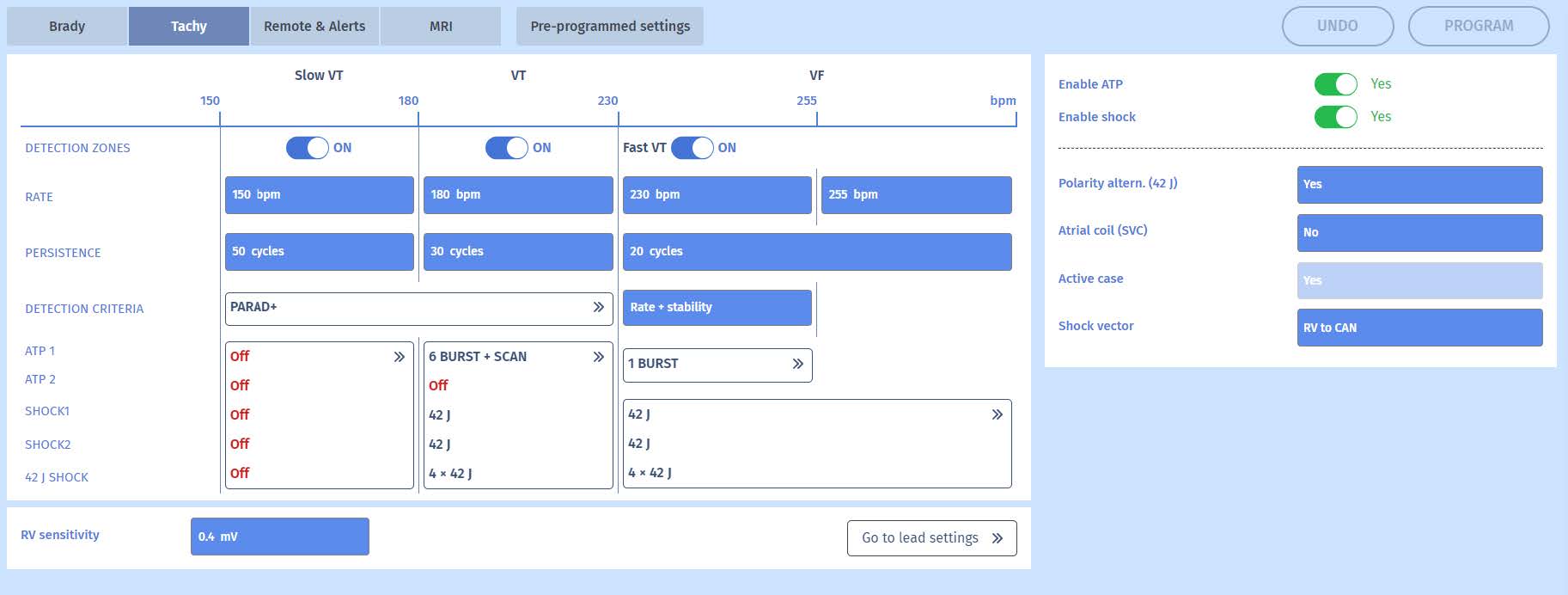
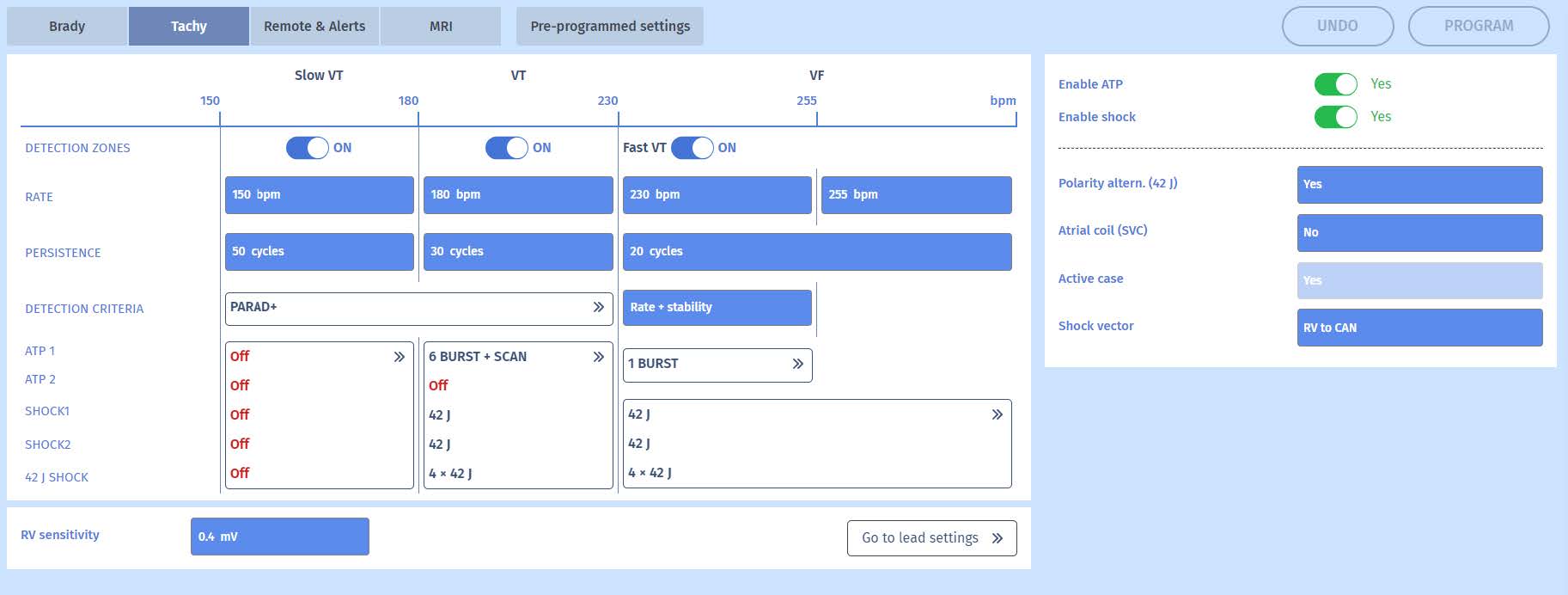
Programming

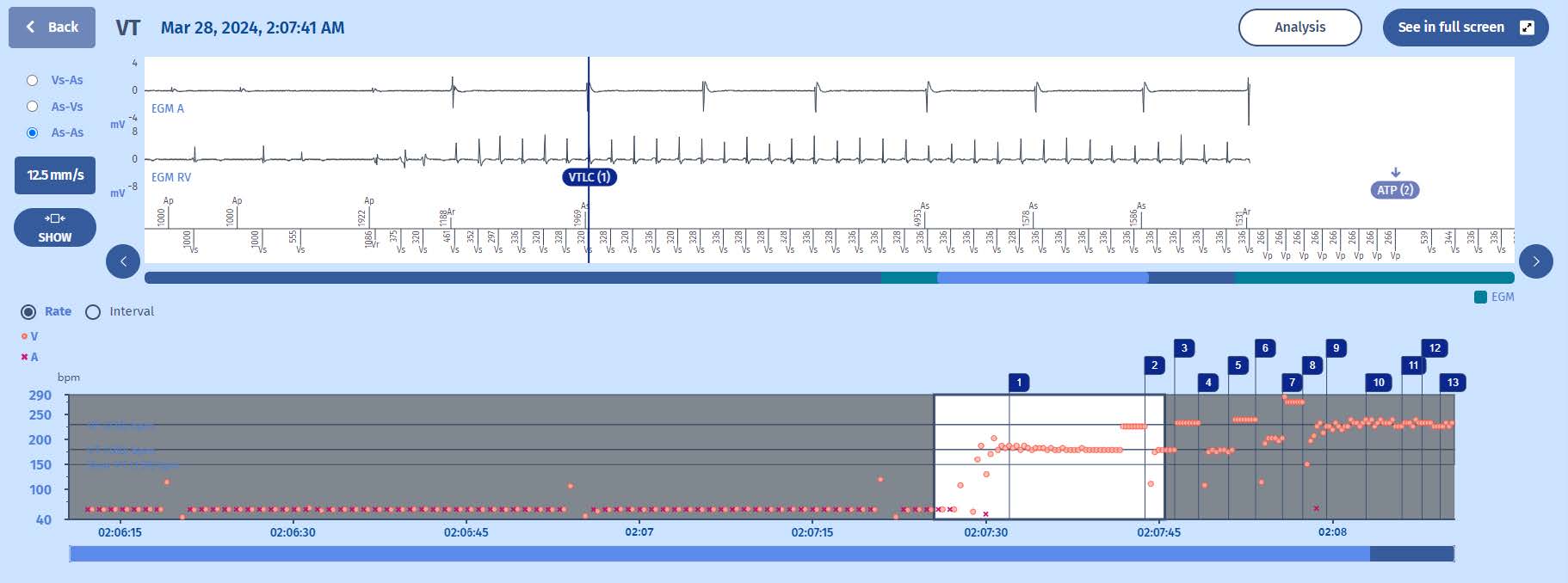
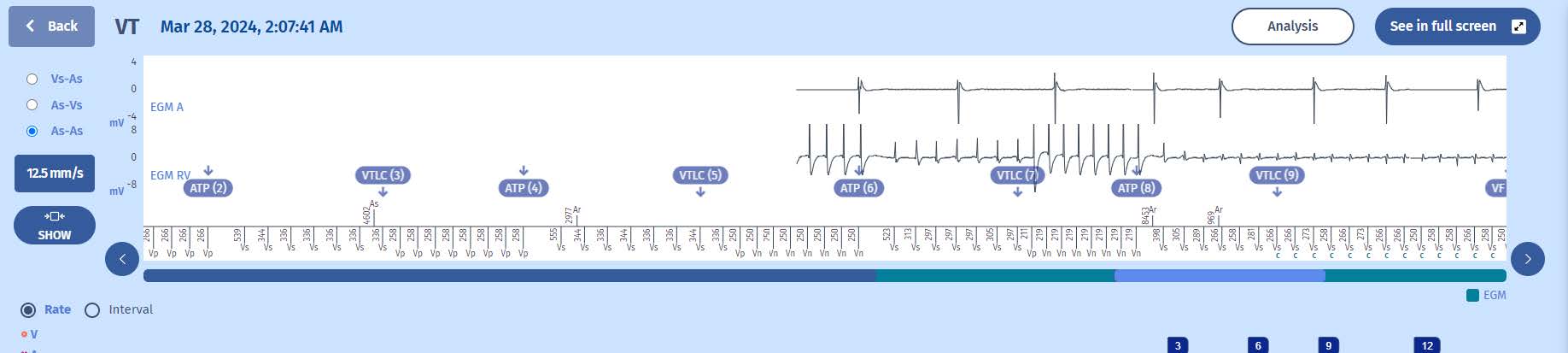
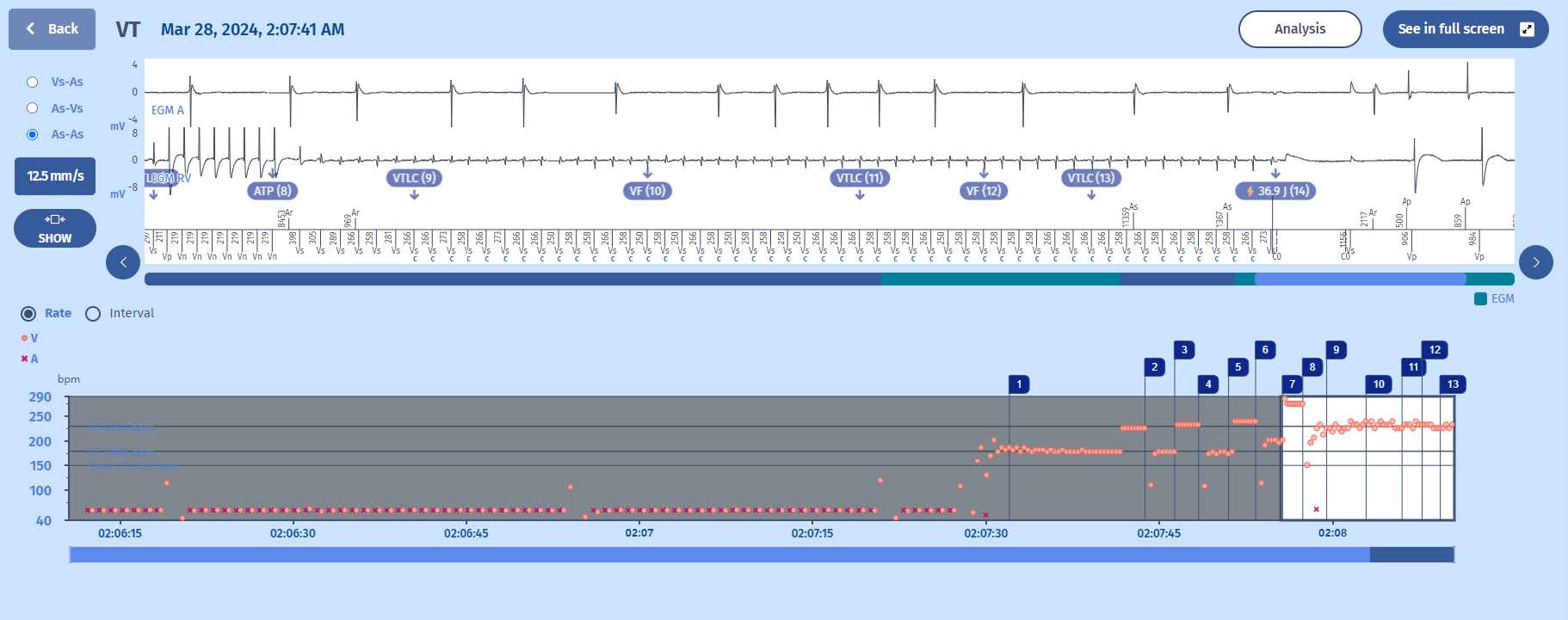
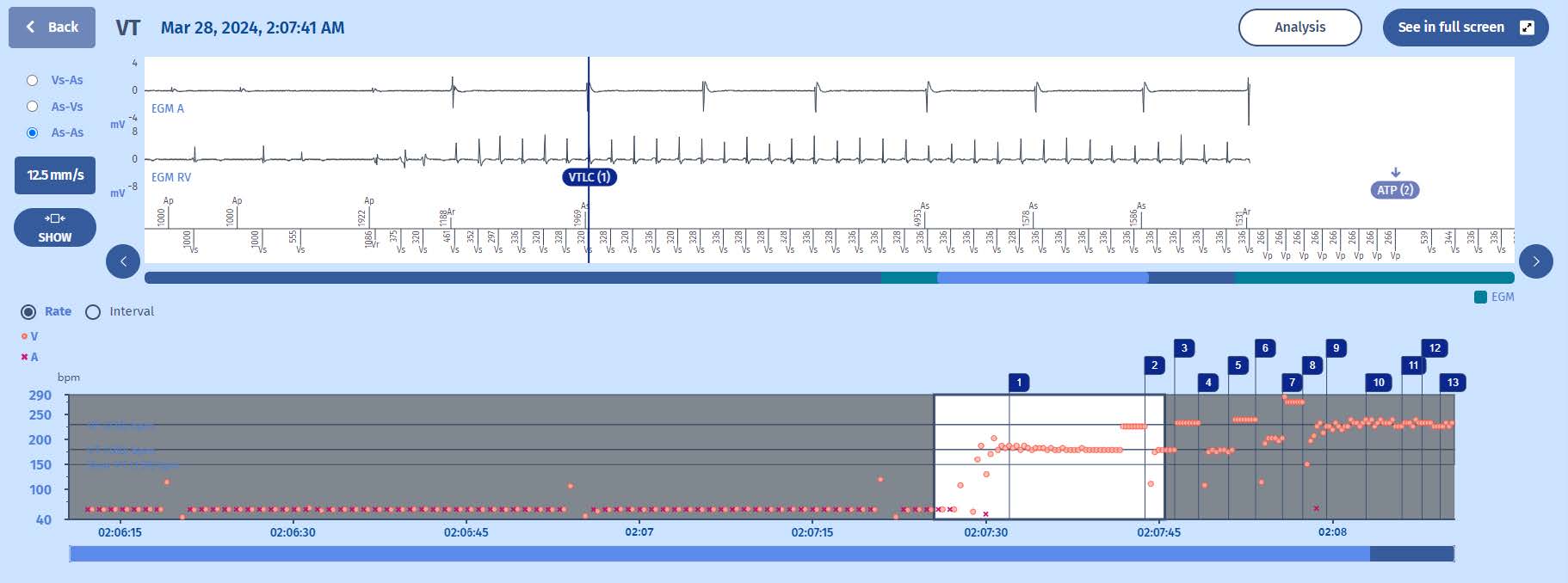
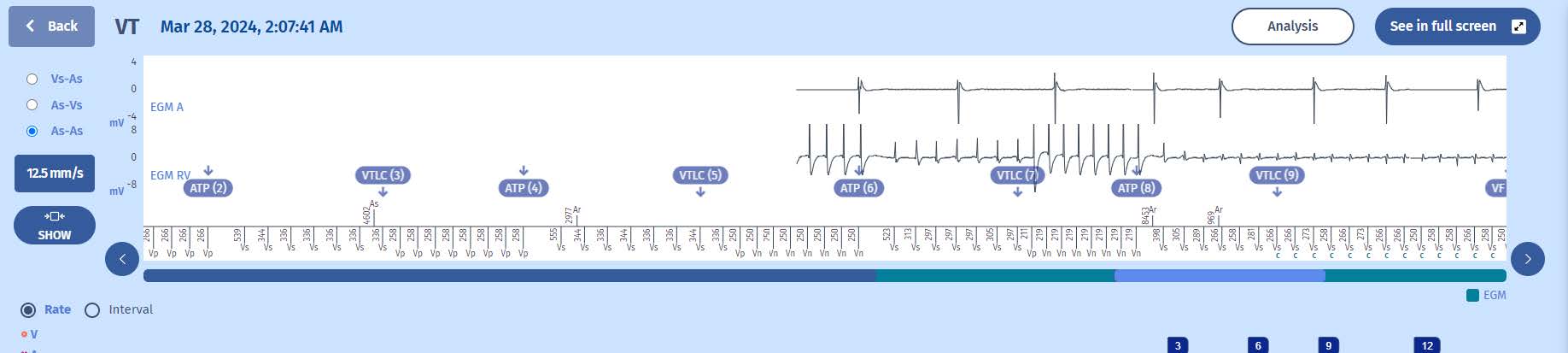
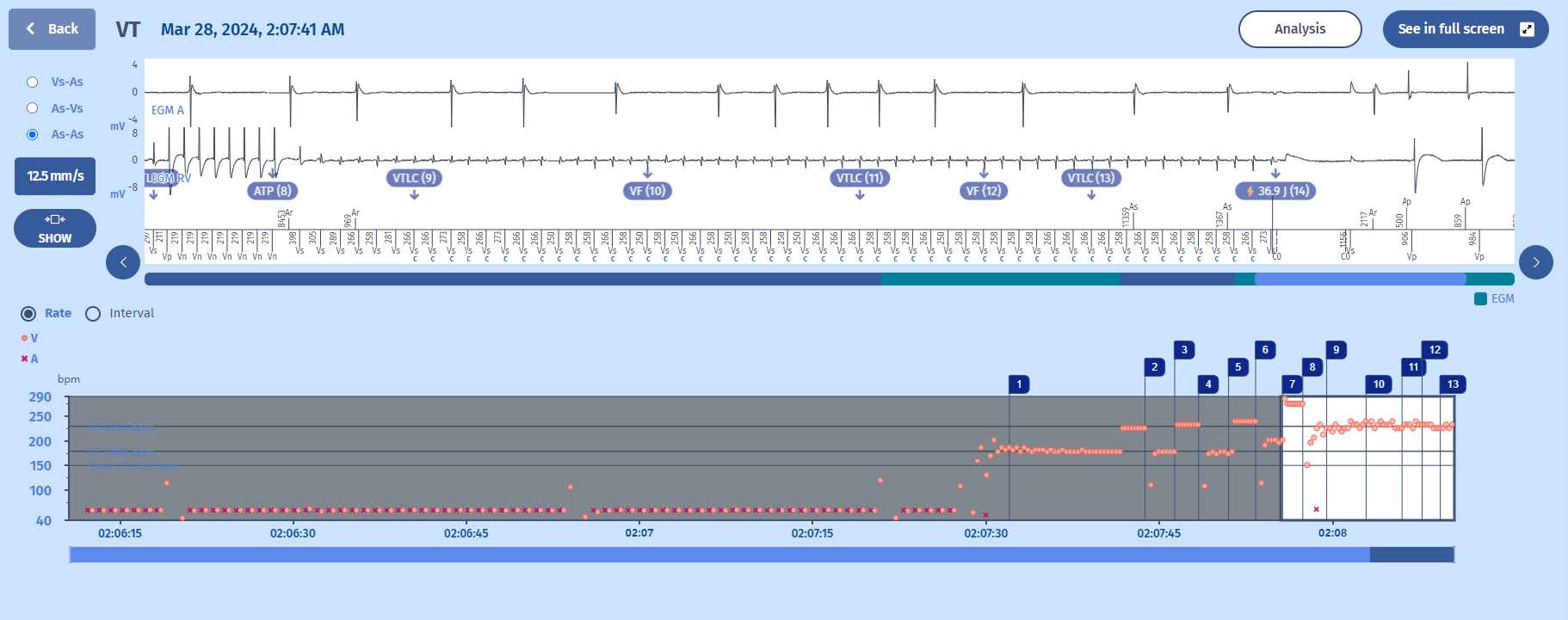
EGM
Explanation
This clinical case illustrates the escalation of the applied therapies according to the zones in which the tachycardias are located, and according to their transition from one zone to another.
- The episode starts with a stable rhythm at 60 bpm when suddenly there is an acceleration of ventricular cycles into the VT zone (>180/min).
- On the EGM we can clearly see that it is a monomorphic ventricular tachycardia with cycles around 330 ms. The diagnosis is made and the persistence is filled.
- The first therapy is an ATP (burst) which does not terminate or alter the VT.
- There is redetection of the VT (marker: VTLC 3) with another non-efficient ATP(4)
- There is again re-detection of the VT with another burst
- Notice that while the VT cycle length remains the same, the bursts accelerate slightly every time. This is due to programming of BURST + SCAN with a decrement of 8 ms for every sequence.
- The third ATP (marker: ATP 6) accelerates the VT, the cycles going from >330 ms to <300 ms but they are still in the VT zone with delivery of a fourth burst at the shortest possible cycle length; 220 ms.
- The fourth ATP again accelerates the VT with cycles as short as 258 ms
- The fourth ATP sequence was delivered with all cycles at the “minimum ATP cycle length.” This causes the ATP program to terminate (interrupt). Therefore,the next therapy is a shock, the ICD start charging.
- During the charge the VT cycles straddle between the VT zone and the VF zone
- At the end of the charge the majority is VT and the persistence is still full (not reset by VF majorities).
- The delivered therapy is the first shock in the VT zone which terminates the VT.
- Slow rhythm is quickly declared after 6 cycles outside any tachy zones (and not following blanking).
Discussion
The ICD will apply therapies depending on the zone in which it is detected at the end of its persistence.
- For the Slow VT/VT transition, when the tachycardia rate accelerates and enters the upper zone with the average of the last 4 persistence cycles in this upper zone, it is the therapy of the upper zone which is applied; similarly, if, when
slowing down, the tachycardia enters the lower zone with the average of the last 4 persistence cycles in this lower zone, it is the therapy of the lower zone that is applied «i.e. the therapy with equal or higher level of aggressiveness
(all ATP programms have the same level whatever the Slow VT or the VT zone).»
- For the VT/VF transition, when the tachycardia rate accelerates and enters the upper zone (FVT/VF), the majority rhythm will change from VT to VF and 60 after the counting of the FV persistence, it is the therapy of the upper zone that is applied; similarly, if, when slowing down, the tachycardia enters the lower zone (VT), it is the higher or equal therapy in terms of level of aggressiveness that will be applied, the FVT/VF ATP being considered « stronger » than the VT/Slow VT ATP.
- After a therapy, and in redetection, the same diagnosis as determined before the therapy increments the persistence counter and triggers the therapy planned in the program; if the diagnosis changes from VT to VF, a new VF persistence counter is restarted.
- In this case we see that ATP accelerates the rate but as we remain in the same zone (VT), we will still apply another ATP. However even when the VT again accelerates and remains in the VT zone, the ATPs are limited at 220 ms (programmed ATP Minimum cycle length) and no longer deliverable. It is a shock which terminates this VT in the VT zone.
- The escalation of therapies, i.e. the progressive aggressiveness from one therapy to another in case of perpetuation of the tachycardia, applies in a same zone. It also applies from one zone to another: if the ATPs have been exhausted in a zone and the tachycardia changes zone, i.e. an upper zone or a lower zone, the called-upon therapy will necessarily be the next line programmed therapy in the new zone.
Are ATPs more dangerous than they are efficient?
As ramps are more aggressive than bursts (shorter pacing intervals), they are considered as more arrhythmogenic by most. However, in our study with over a 1000 confirmed VT episodes, we found no difference between burst and ramp arrythmogenicity or
efficacy. Read the full article in Heart Rhythm or download the PDF here. Also we found that the first burst (for any VT) is 63% efficient with low acceleration rate. As multiple ATPs are delivered, the chance of success increased but also the risk of
acceleration. After the 6th ATP, new ATPs are unlikely to be effective. Delivering 6 ATPs terminates the VT in >80% of cases. While we cannot deny the risk of acceleration, the alternative has the same outcome: delivery of a shock.
Take home message
Antitachycardia pacing may accelerate a monomorphic ventricular tachycardia into a faster VT or even VF.
Multiple ATPs decrease the risk of shocks, even though there is a slight risk of acceleration requiring shock(s).