A 66-year-old man, implanted with a dual-chamber defibrillator for secondary prevention due to ischemic heart disease in the absence of infarction, with an ejection fraction of 27%, presenting initially with decompensated heart failure with narrow QRS complexes. The patient came in for a consultation because he had experienced an electric shock preceded by palpitations and presyncope.
Summary screen
Here is the first screen when interrogating the defibrillator:
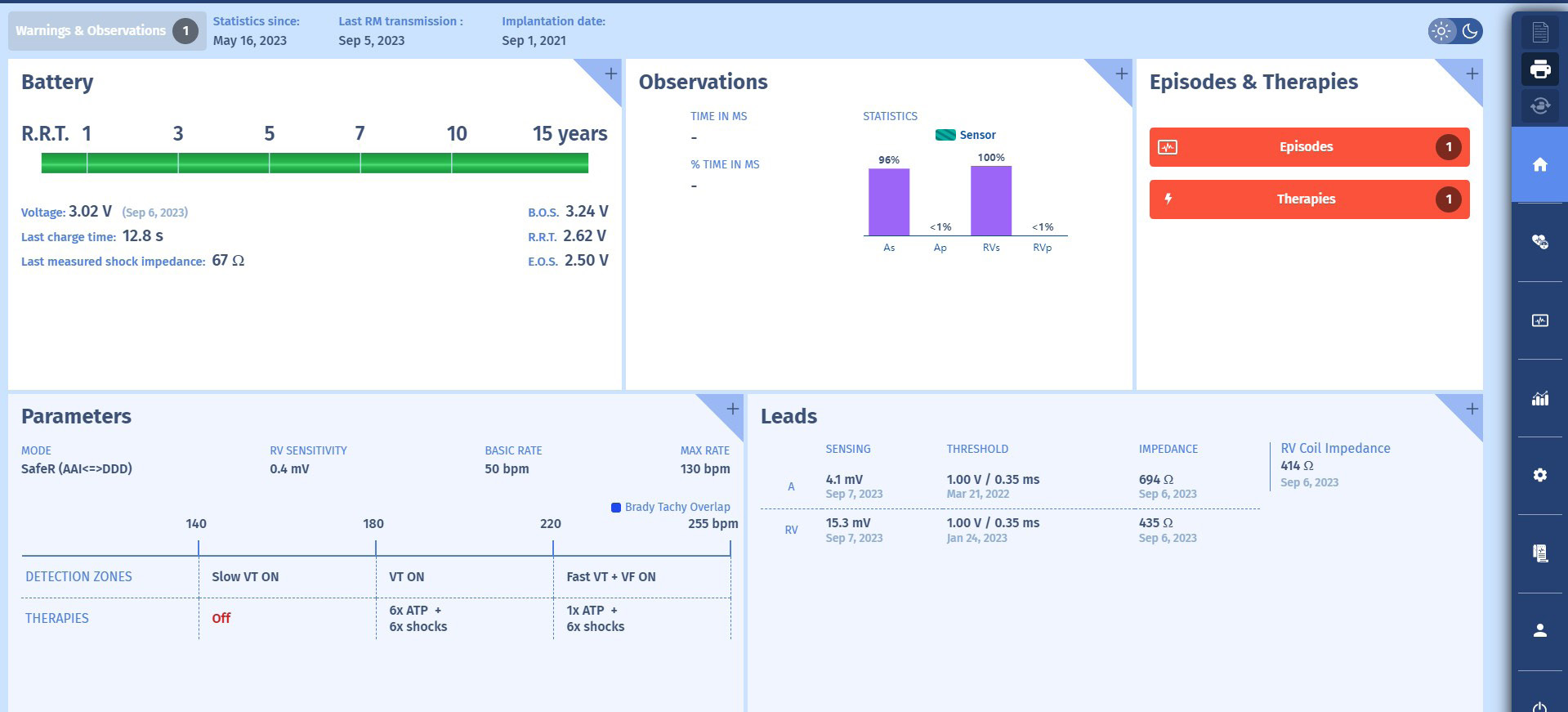
Interpretation
1 At interrogation, and after verification of the leads, we can see that they function perfectly, that the battery is new, that the patient has received at least one shock since the shock impedance was measured, with a value of 67 Ohm. The anti-bradycardiaprogramming attempts to abide to AV conduction by the SafeR-R mode; the ventricular pacing rate is <1%. For tachycardias, a Slow VT zone, from 140 to 180/min, is a monitoringzone; between 180 and 220, a VT zone with therapies comprised of 6 ATPs and 6 shocks (all at maximum energy of 42 Joules not visible on this screen); above 220/min, a Fast VT zone + VF, with up to 255/min, 1 pre-shock burst if the tachycardia is stable, followed by maximum energy shocks, and maximum energy shocks alone beyond 255/min. The programming is in keeping with recommendations.
2 In the Observations section, there was no mode switch, suggesting the absenceof atrial rhythm disorders, especially since the atrial detection in sinus rhythm is very good (4.1mV), suggesting a good detection of AF when occurring (simple)presumption since there is limited correlation between the amplitude of the sinus signals and the atrial arrhythmia signals).
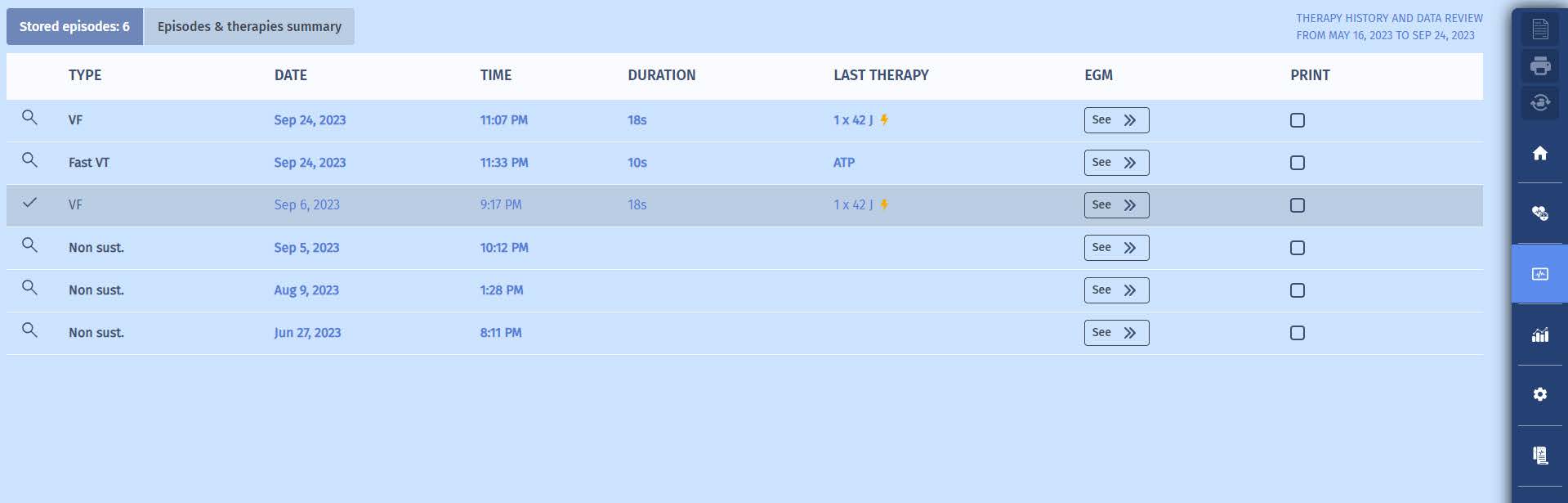
3 In the Episodes & Therapies section, we can that there has been 1 episode with therapies. On the old user interface, there would have been more information presented in the form of a table. But for the sake of clarity, it has been decided toconsolidate this information and present the details elsewhere. When we click on one of those red buttons (or when we go to the “episodes” screen we willaccess the following episode list. The list of memorized episodes appears with their respective
type, date, duration and treatment applied.
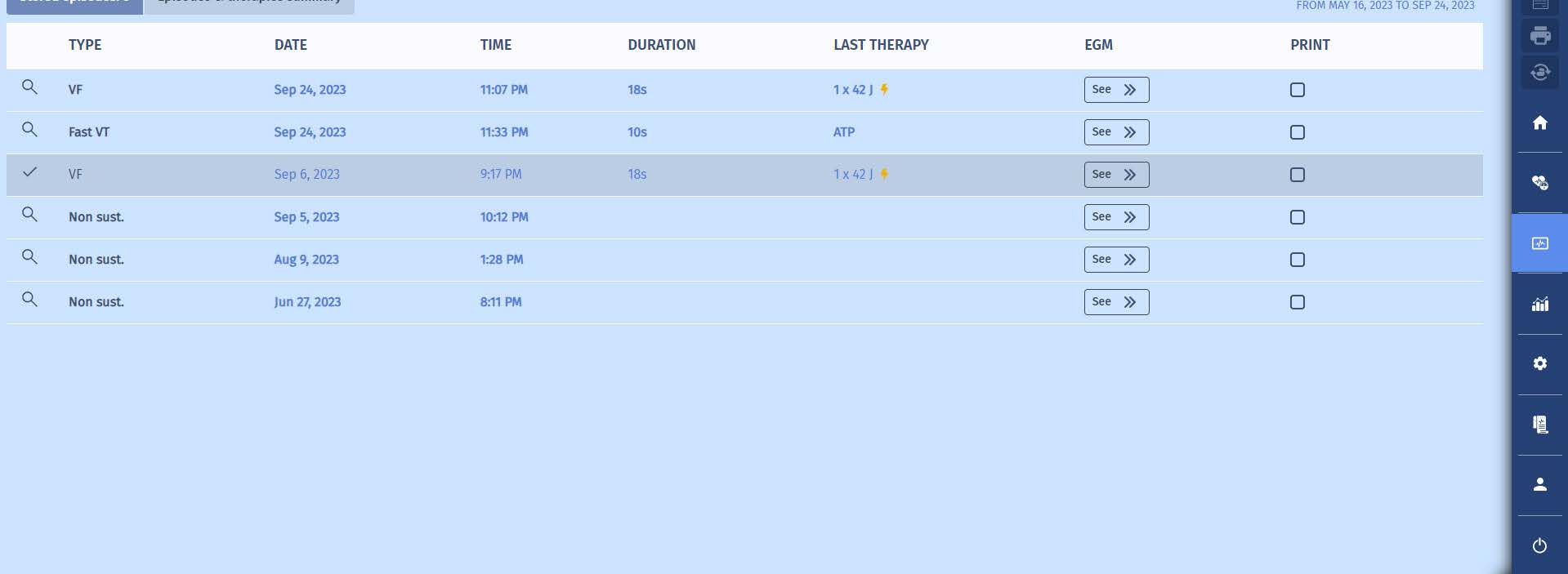
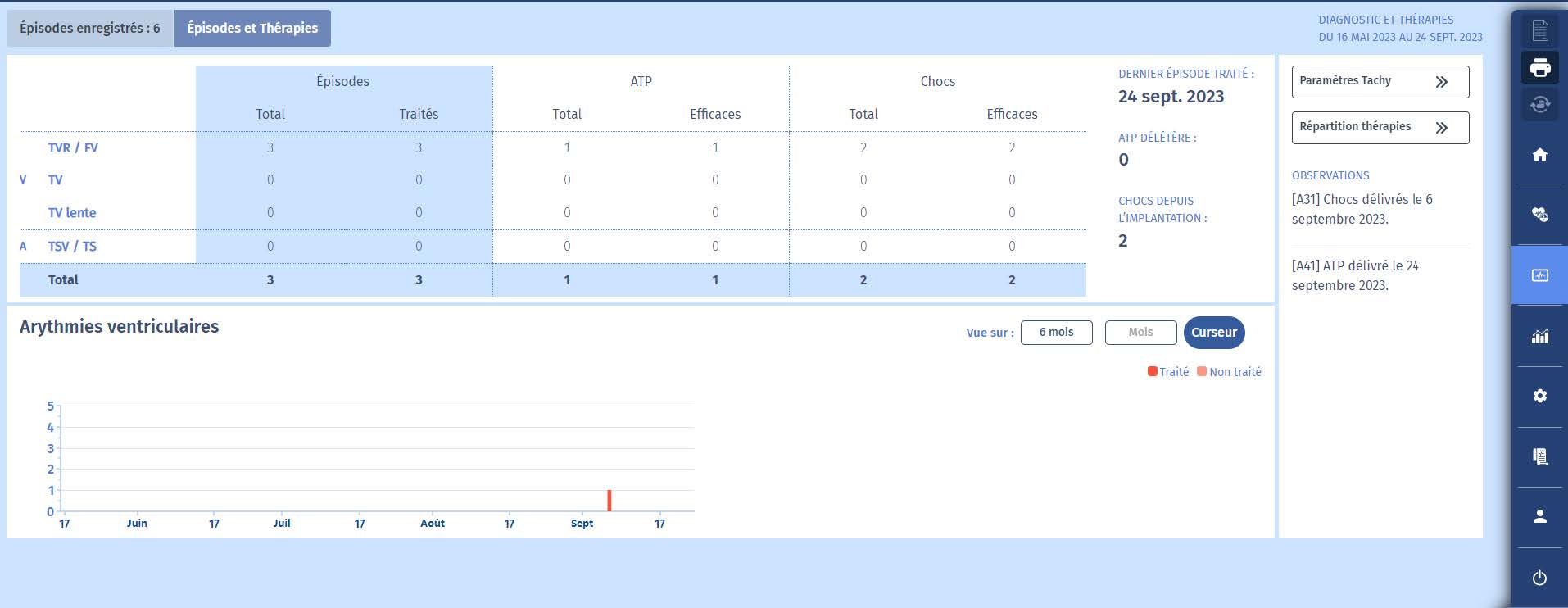
When we click on “Episodes and Therapies summary”, we can observe an table with episodes and treatments. We can see that there has been 1 VF episode with treatment.
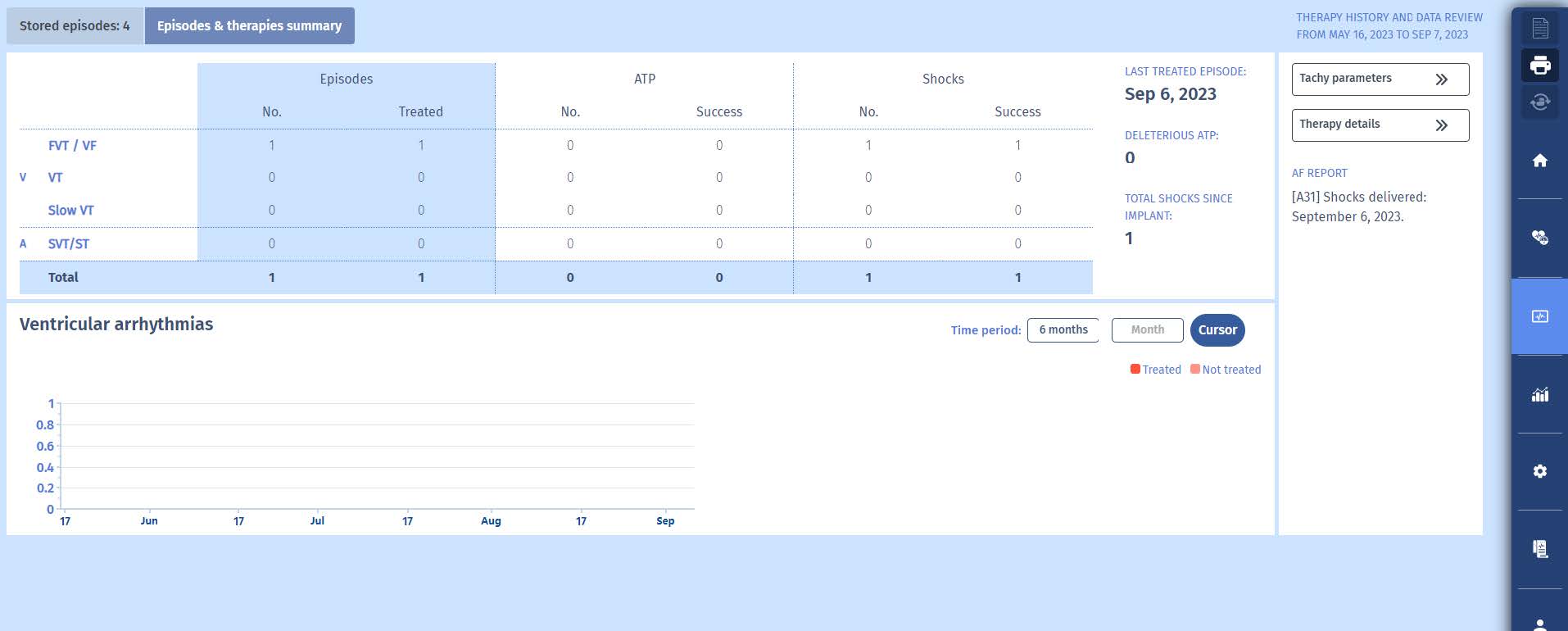
Episode review
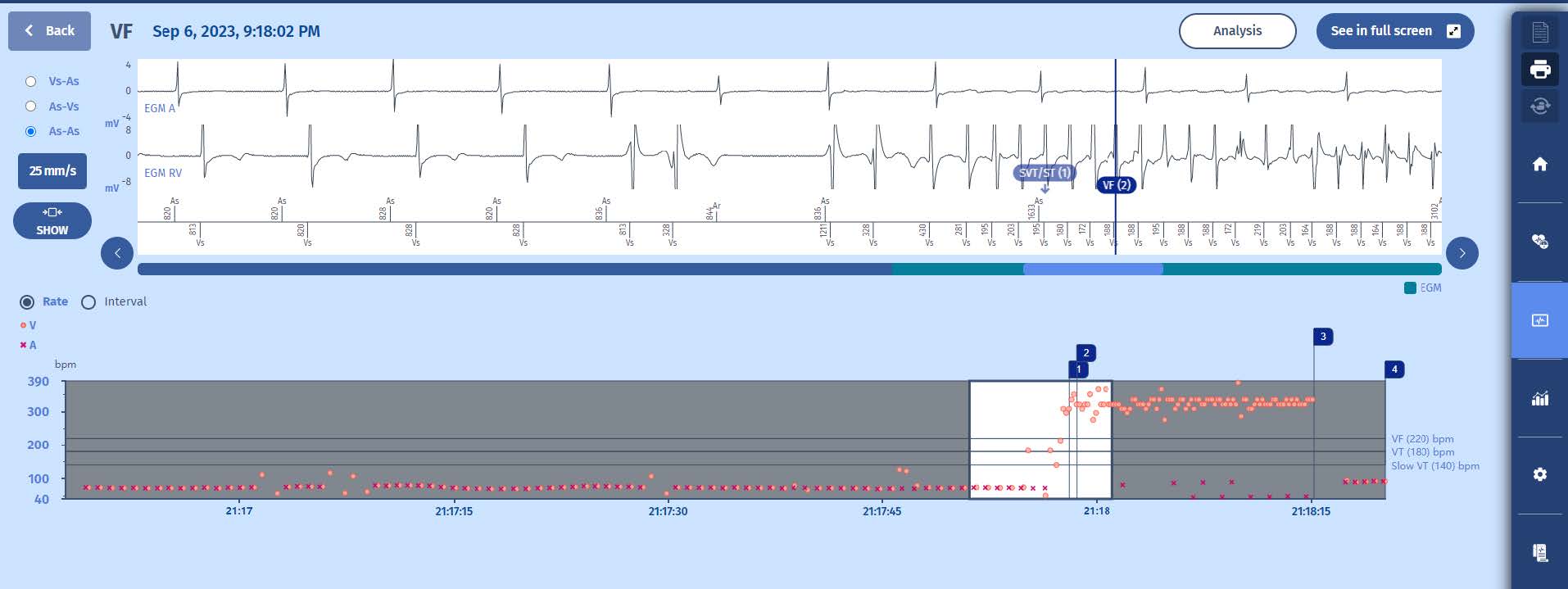
Let’s review the most recent episode, diagnosed as VF, resulting in a shock. We will get a combined screen showing the EGM corresponding with the highlighted area on the tachogram displayed below.
Interprétation
1 A l’interrogatoire, et après vérification des sondes, on constate qu’elles fonctionnent parfaitement, que la pile est neuve, que le patient a reçu au moins un choc depuis que l’impédance de choc a été mesurée, avec une valeur de 67 Ohm. La programmation antibradycardie tente de respecter la conduction AV par le mode SafeR-R ; la fréquence de stimulation ventriculaire est <1%. Pour les tachycardies, une zone de TV lente,de 140 à 180/min, est une zone de surveillance ; entre 180 et 220, une zone de TV avec des thérapies composées de 6 ATP et 6 chocs (tous à l’énergie maximale de 42 Joules non visible sur cet écran) ; au-delà de 220/min, une zone de TV rapide +FV, avec jusqu’à 255/min, 1 burst de pré-choc si la tachycardie est stable, suivi de chocs à énergie maximale, et des chocs à énergie maximale seuls au-delà de 255/ min. La programmation est conforme aux recommandations.
2 Dans la section Observations, il n’y a pas eu de changement de mode, ce qui suggère l’absence de troubles du rythme auriculaire, d’autant plus que la détection auriculaire en rythme sinusal est très bonne (4,1 mV), ce qui suggère une bonne détection de la FA lorsqu’elle se produit (simple présomption puisqu’il y a une corrélation limitée entre l’amplitude des signaux sinusaux et les signaux d’arythmie auriculaire)
3 Dans la section Episodes et thérapies, nous pouvons voir qu’il y a eu 1 épisode avec des thérapies. Sur l’ancienne interface utilisateur, il y aurait eu plus d’informations présentées sous la forme d’un tableau. Mais par souci de clarté, il a été décidé de consolider ces informations et de présenter les détails ailleurs. En cliquant sur l’un de ces boutons rouges (ou en accédant à l’écran “épisodes”), nous accédons à la liste d’épisodes suivante. La liste des épisodes mémorisés apparaît avec leur type, leur date, leur durée et le traitement appliqué.
Lorsque nous cliquons sur “Résumé des épisodes et des thérapies”, nous pouvons observer
Revue d’épisodes:
Examinons l’épisode le plus récent, diagnostiqué comme une FV ayant entraîné un choc. Nous obtiendrons un écran combiné montrant les EGM correspondant à la zone mise en évidence sur le tachogramme affiché ci-dessous.
The tachogram reveals the following elements:
1 On the right of the graph, the following zones are noted: a monitoring Slow VT zone from 140 to 180/min, a VT zone from 180 to 220/min with bursts, ramps and shocks, and VF above, with a FVT zone from 220 to 255/min with 1 burst followed by maximum
shocks.
2 Initially, the rhythm is 1:1 in a Slow rhythm zone with some premature ventricular complexes (the higher orange dots) and compensatory pauses (lower orange dots).
3 Suddenly, a chaotic tachycardia occurs in the VF zone. The diagnosis of VF was made (at marker 2), after which a 41.8 Joule shock was delivered (marker 3) with immediate effectiveness.
4 Return to slow rhythm. The episode is terminated (marker 4).
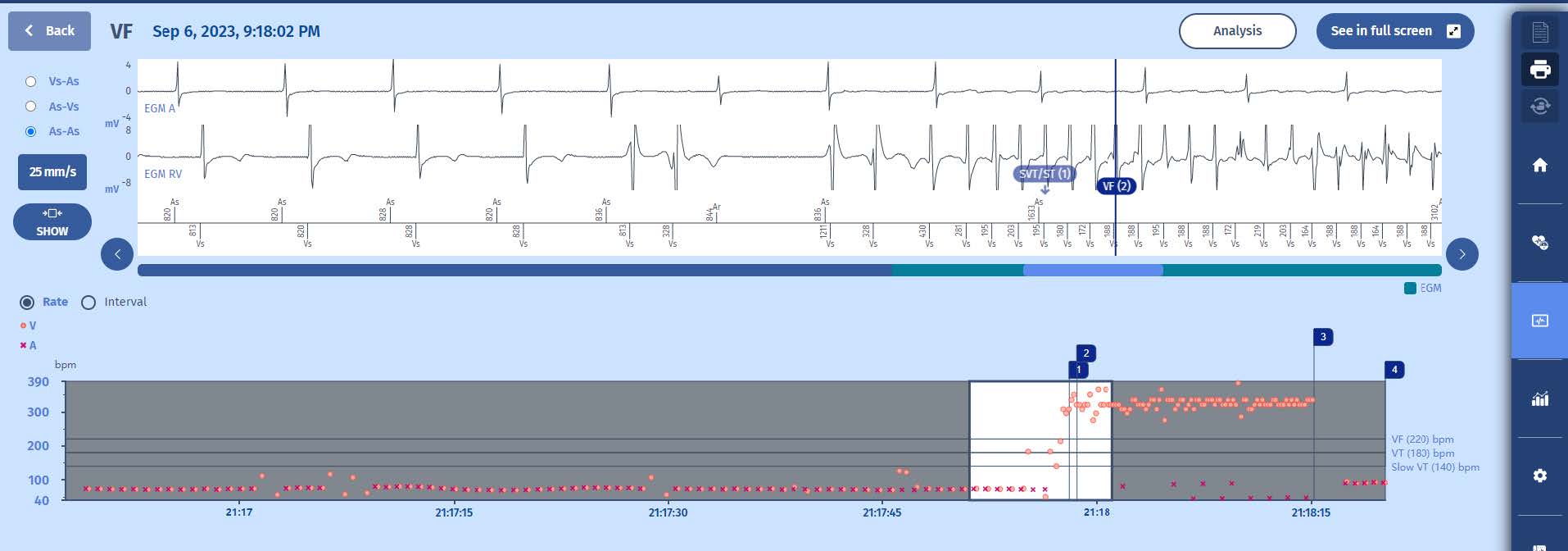
Electrogram: beginning
While the tachygram allows for a quick overview of the episode with possibility of making the diagnosis in most cases, it is essential to analyze the electrogram (EGM) to verify properfunctioning of the ICD. The EGM can be expanded by clicking on « See in full screen ».
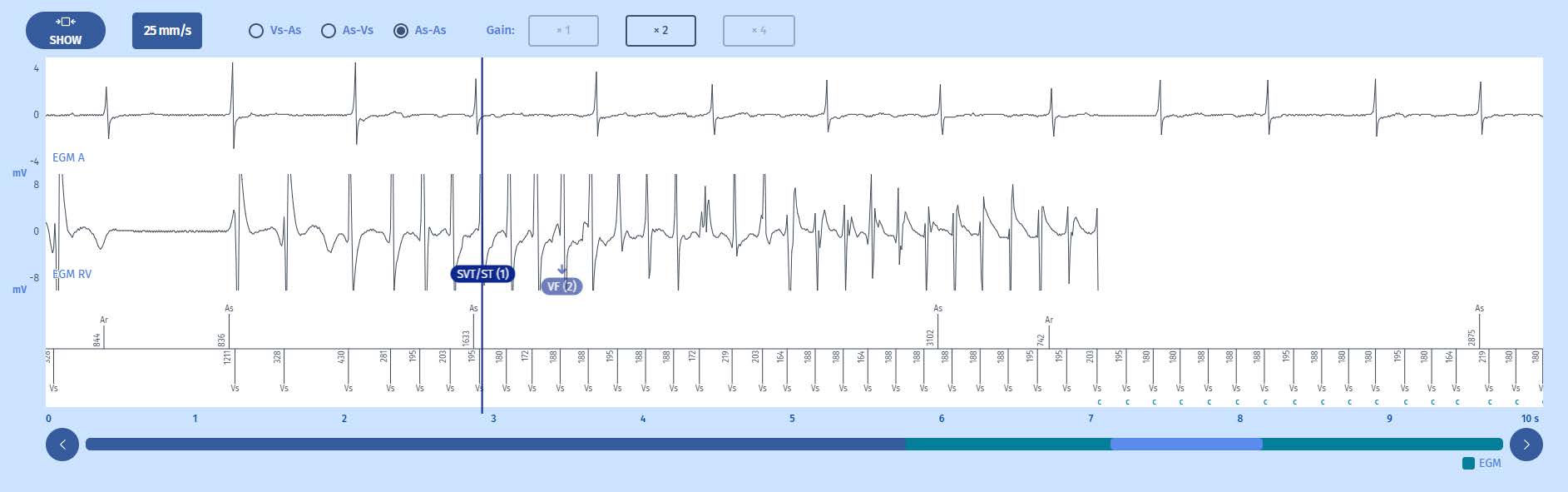
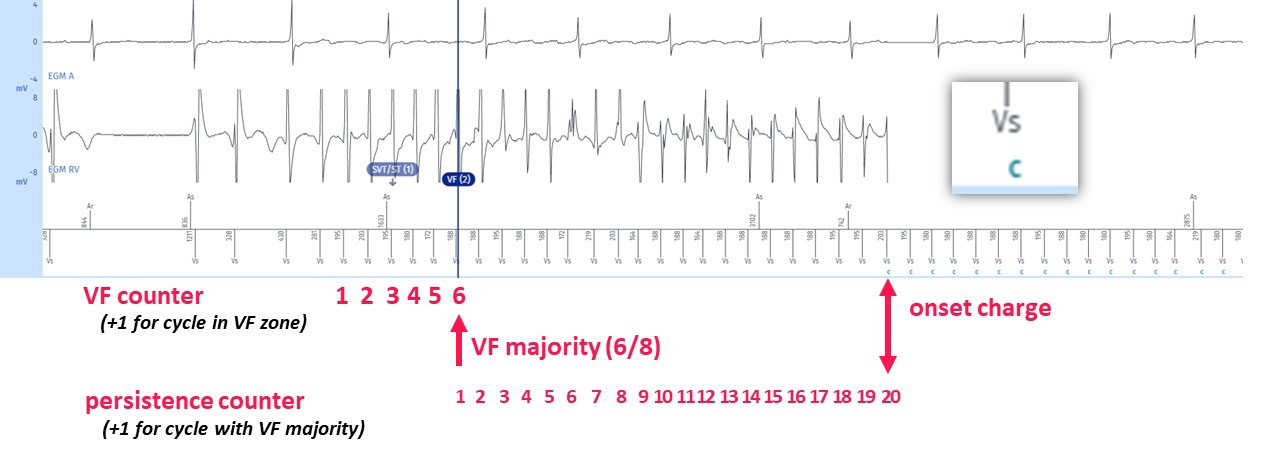
Tracings: The tracing at the top entitled EGM A is the atrial electrogram, the tracing underneath entitled EGM RV is the ventricular electrogram, lastly, at the bottom, the atrial markers above the line and ventricular markers below, along with the time intervals. The gain can be changed at the top (now set at X 2). The running speed can also be changed, ranging from 12.5 to 100 mm/sec.
The EGM shows the following elements
1 An intrinsic rhythm with spontaneous atroventricular conduction rhythm at baseline;
2 A few ventricular extrasystoles which seem to be associated with the onset of a polymorphic tachycardia above 220/min, perfectly detected, with a slow and regular atrial rhythm, and small amplitude signals on the atrial channel which are far-field signals of ventricular origin and not detected by the atrial chain;
3 After 6 out of 8 cycles in the VT zone, the diagnosis of SVT/ST is made (marker 1); this is often seen in VF episodes and is caused by the “warming” up of many ventricular arrythmias. The combination of fast cycles (PVCs and the onset of VF) and slow cycles (compensatory pauses or differences in cycles often seen during “warming up” period) results in the VT criteria being fullfilled before the VF criteria. As the rythm is unstable, it is considered SVT by the discrimination algorithm, therefore we see a first marker
SVT/ST, rather than VT of VF.
4 After a majority of 6 out of 8 cycles in the VF zone, the diagnosis of VF is made shown by the marker VF (2). It should be pointed out, even before the course on discrimination, that the discrimination criteria (PARAD+) are not active because it is the VF zone.
5 After diagnosis of VF, treatments are not directly delivered as we want to give the tachycardia the chance to self-terminate. The tachycardia needs to complete the persistence counter before therapies are delivered. After 20 persistence cycles, as programmed (and as recommended), during which the diagnosis of VF is confirmed at each cycle, according to the 6/8 majority, the capacitor charges (« C »). Indeed, no burst was triggered because the rate is above the 220 – 255/min zone. (If the tachycardia
had been within this aforementioned zone, and if it had been stable, then a burst would have been triggered. If the tachycardia had been within this zone but conversely unstable, then an immediate shock would have been delivered without a prior burst).
Electrogram: end
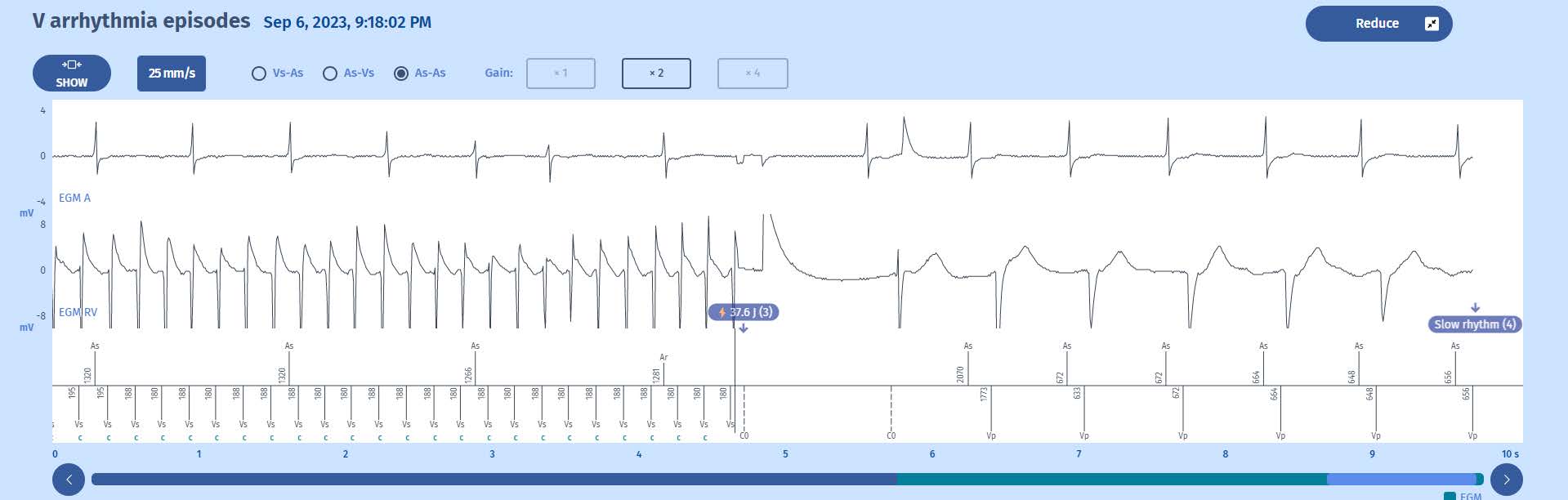
1 Once charged, the defibrillator sends a shock on the next cycle which is in the VF zone; shown by the marker: 37.6J (3).
2 After the shock, there is a 1-second blanking period (between C0 markers). After six cycles out of tachycardia zones the Slow rhythm majority is met (6/8) and the episode is terminated.
Comments
The EGMs show normal functioning of the defibrillator. The counting of the events is carried out as follows:
1 Each ventricular cycle detected outside refractory periods is classified as: Slow, VT or VF, depending on the programming of the tachycardia zones.
2 In a sliding window of 8 cycles and for each cycle, the device classifies RR cycles with a 16-ms margin in a histogram. Paced cycles do not enter into the constitution of the histogram.
3 In the present case, 75% of the 8 cycles, hence 6, must be in the VF zone for the diagnosis to be established. For a therapy to be triggered, it is necessary that the persistence of the programmed number of cycles is fulfilled (in this instance 20 cycles, according to the recommendations), with the VF majority detected for each cycle. The last 4 cycles determine the initiation of therapy due to FVT or VF: each of the last 4 cycles are analysed and if any of the latter is in the VF zone above the FVT zone, the
assigned therapy will be a 42 J shock (depending on the programming), and the charge of the capacitors begins.
4 All tachycardia cycles are in the VF zone during the charge which is therefore continuous. It is on the ensuing cycle which follows the end of the charge and which is in VF zone that the shock is delivered.
5 After the shock, 6 out of 8 cycles are in the Slow zone, the rhythm is deemed slow and the episode is terminated.
A systematic approach must be used to read the follow-up data:
1 Make sure that the leads are working properly and repeat the tests systematically. Leads in perfect condition report reliable signals to the defibrillator and the stored data are interpretable. If the leads do not work properly, the reading of the memories will need to be with much more caution.
2 Make sure you analyse the programming of the device properly to correctly interpret the memories. The device only records events according to what it is asked to do and record !
3 To correclty interpret EGMs, a sound knowledge of the programmed algorithms is required.