A 72-year-old man with a triple-chamber defibrillator for dilated heart disease with healthy coronary arteries, an ejection fraction of 28%, complete left bundle branch block, and optimal medical therapy. The patient has never experienced a VT until now, and is
known with paroxysmal AF. The patient consults due to a loss of consciousness the day before.
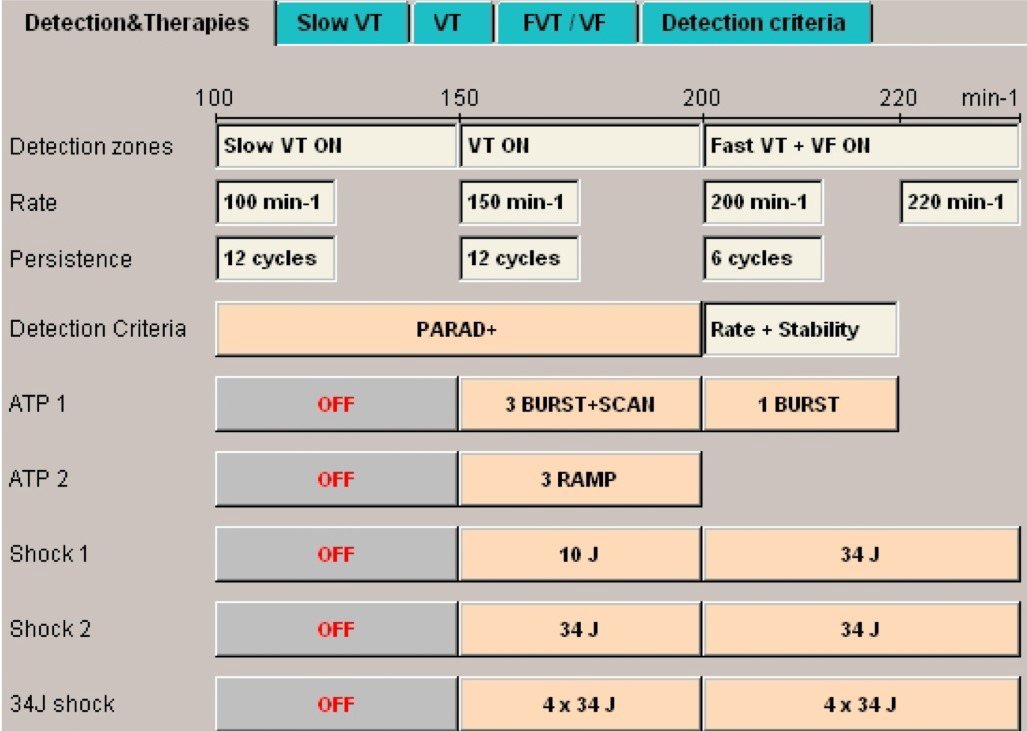
Programming
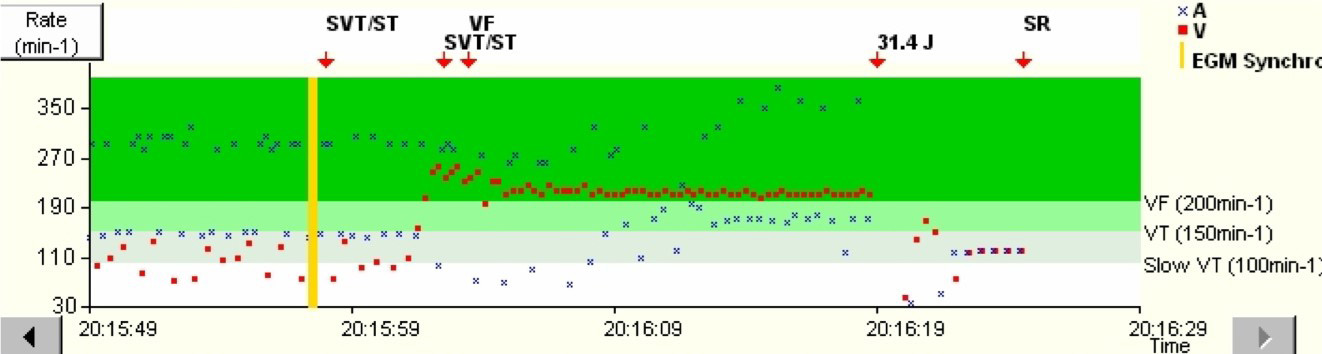
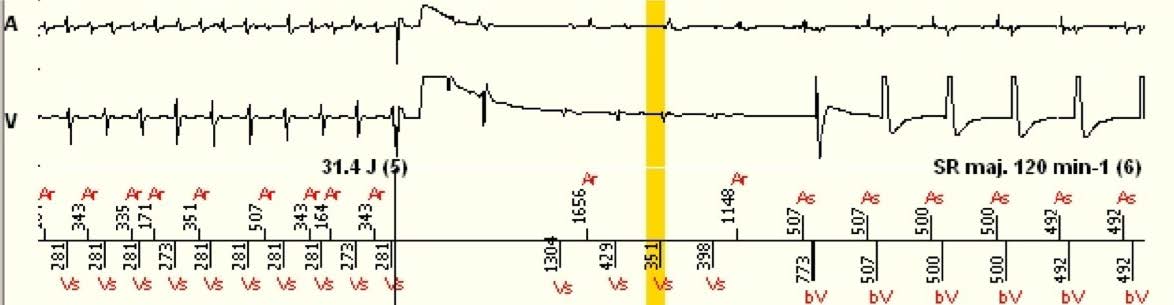
Interval plot
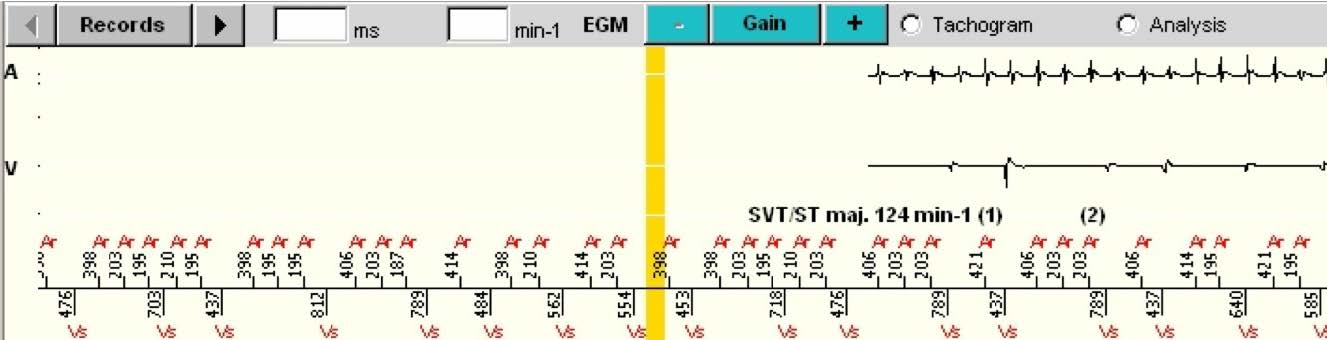
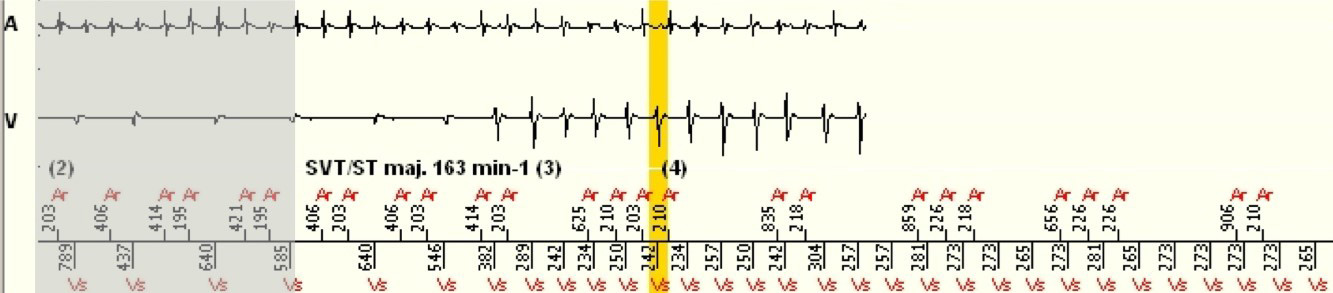
The shaded areas are the portions of the EGM that are the repetitions of the end of the previous image.
Interpretation
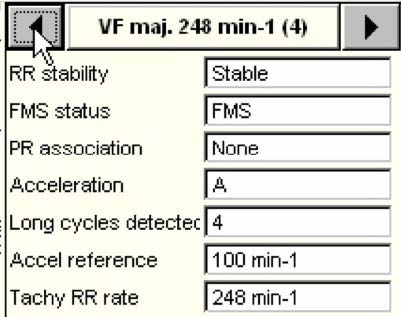
No discrimination when the tachycardia is in the VF zone (Fast VT zone included). The stability criterion in the Fast VT zone is only used to decide whether or not to deliver an ATP before the charging of the capacitors. Inducing and terminating a VF with a shock test in a non-anticoagulated AF patient is contraindicated if the absence of intracardiac thrombosis is not verified, and a flash anticoagulation has not been administered.