Medtronic - Management of atrial arrhythmias
Content
Mode switch due to atrial arrhythmias
Switching to asynchronous mode (new pacemaker platform)
The pacemaker switches to DDIR mode (non-programmable mode) when the sudden onset of AT/AF criterion is met if the median value of the 12 most recent detected atrial intervals is shorter than the programmed AT/AF interval and if the AF evidence counter (2 atrial signals detected between 2 ventricular signals) is greater than or equal to 3. To avoid a sudden drop in ventricular rate, it very gradually reduces the pacing rate from the synchronous atrial rate to the rate indicated by the sensor over several pacing cycles. Event markers include an “MS” marker for each mode switchover, whether to asynchronous or synchronous mode.
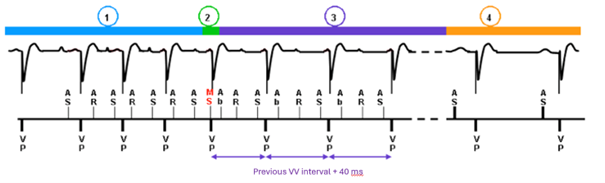
- Onset of atrial arrhythmia with acceleration of stimulated ventricular rate
- The criterion for sudden onset of AT/AF is met; MS (mode switch) marks the transition to fallback mode; transition from programmed pacing mode to DDIR mode
- Gradual transition from rapid ventricular pacing rate to servo-controlled rate (+40 ms at each interval)
- End of arrhythmia; return to programmed mode (except for MVP mode, for which there is always a return to DDD before a return to AAI)
Switch to atrial follow-up synchronous mode (new pacemaker platform)
The episode ends when a normal sinus rhythm (or normal paced rhythm) is identified for 5 consecutive ventricular intervals, or if the median atrial interval is greater than the AT/AF detection interval, or if the AT/AF counter is less than 27 for 3 minutes.
Recording episodes of atrial arrhythmia
Pathological atrial events are recorded when they cause a refractory period. It is possible to view the graph, EGMs, and a summary text for different recorded episodes.
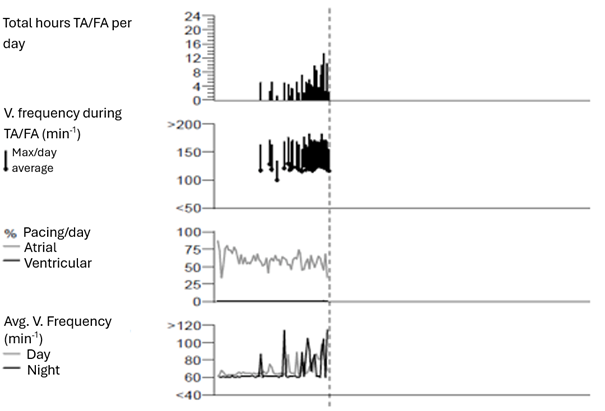
The cardiac monitor report provides information on AT/AF episodes and ventricular rhythms, indicates the time spent in AT/AF, and provides information on the evolution of total AT/AF hours per day (graph).
Flutter management in Medtronic
Algorithm for detecting masked flutter
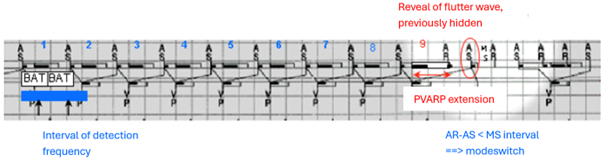
This algorithm searches for the presence of an atrial signal that is not seen because it falls within the atrial blanking period after ventricular pacing when:
- there is a succession of rapid AS-VP cycles
- there are 8 consecutive AS-AS intervals that are less than twice the sum of the AV delay + post-ventricular stimulation atrial blanking and less than twice the interval corresponding to the atrial arrhythmia detection rate.
In this case, on the 9th cycle, the algorithm increases the PVARP to bring the next atrial event (AR) into the refractory period, not stimulate the ventricle on a beat, and unmask the next flutter wave (AS), which is no longer hidden in the post-ventricular stimulation atrial blanking.
This algorithm was present on older pacemaker platforms where post-ventricular atrial blanking was absolute. It should be noted that on newer platforms, post-ventricular atrial blanking is no longer absolute (when the PVAB is programmed to partial or partial+), and that a signal falling within the blanking period is counted for the diagnosis of arrhythmias, which limits the usefulness of this type of algorithm.
AF prevention algorithm in Medtronic
Non-competitive atrial pacing
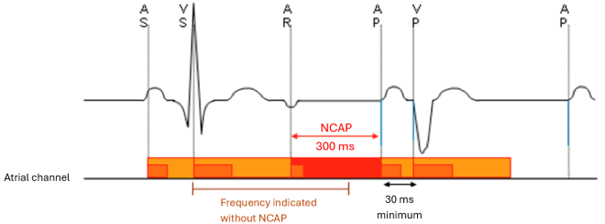
Atrial arrhythmia may be initiated if a paced atrial event occurs during the vulnerable period of the atrium. Non-competitive atrial pacing (NCAP) is designed to prevent the initiation of atrial arrhythmia by pacing during the relative refractory period of the atrium.
When NCAP is programmed to On, a refractory atrial event detected during the PVARP triggers a programmable NCAP period during which no atrial pacing can occur.
When atrial pacing is delayed by NCAP operation, the pacemaker attempts to maintain a stable ventricular rate by reducing the subsequent stimulated AV delay. However, it does not shorten the stimulated AV delay to less than 30 ms.
The NCAP interval is 400 ms for 1 pacing cycle each time a PVC response or anti-PMT intervention occurs.
Atrial Preference Pacing
Atrial Preference Pacing (APP) is designed to reduce the incidence of atrial tachyarrhythmias by responding to changes in atrial rate by accelerating the pacing rate until a stable pacing rate is achieved that is slightly faster than the spontaneous rate. After each detected non-refractory atrial event, the device decreases the atrial pacing interval by the programmed interval decrement value. Atrial pacing pulses delivered for APP are annotated PP (proactive pacing) on the event marker.
If the next atrial event is another detected non-refractory event, the pacing interval is decremented again. This progression continues until the pacing rate exceeds the spontaneous rate, resulting in a paced atrial rhythm. However, the programmed maximum rate value provides a rate limit for atrial pacing preference. After a programmable period of 100% atrial pacing, the pacemaker gradually decreases the pacing rate in search of the next spontaneous beat. The next sinus beat restarts pacing preference
Atrial Rhythm Stabilization
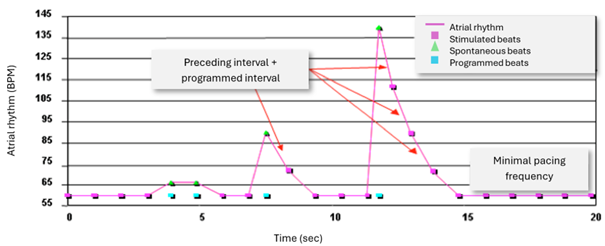
Atrial Rhythm Stabilization (ARS) is a programmable feature designed to prevent sinus pause following a PAC (short-long-short cycle sequences that can cause certain atrial tachyarrhythmias to start abruptly). It responds to an ESA by instantly increasing the atrial pacing rate and then gradually slowing the rate to the spontaneous rate, the programmed pacing rate, or the sensor rate.
When the device is activated by an PAC, it delivers a pacing pulse at the premature interval increased by a percentage of that interval (defined by the programmed Interval Increment Percentage parameter). For each subsequent paced or detected atrial event, the device continues to increase each pacing interval by the programmed percentage of the previous interval. The Maximum Rate parameter sets a limit for ARS. Atrial pacing pulses delivered for ARS are annotated PP (Proactive Pacing) on the event marker.
Post Mode-Switch Overdrive Pacing
Post Mode-Switch Overdrive Pacing (PMOP) is a programmable feature that delivers rapid atrial pacing at the end of a mode switch.
After a mode switch, the device increases the pacing rate beat-by-beat (decreasing the pacing interval by 15 ms per pulse for Adapta and 70 ms for Advisa) until it reaches the programmed rapid pacing rate. It continues DDIR pacing at the rapid rate for the programmed rapid pacing duration. It then regulates the return to programmed atrial synchronous mode by gradually slowing the rate until it reaches the programmed pacing rate, the programmed minimum rate, or the sensor rate.
Response to conducted AF
The response to conducted AF, called ventricular rate stabilization for previous pacemakers, is designed to regulate ventricular rate during AF. The pacemaker modifies the pacing rate beat by beat to pace close to the average intrinsic ventricular rate. Long pauses are eliminated, reducing ventricular rate irregularity. Conducted AF response functions only in asynchronous modes. Therefore, when the device is programmed in DDD or DDDR mode, conducted AF response functions only during a switch to VDIR or DDIR mode. To program conducted AF response to On, mode switching must be set to On.