Single chamber discrimination
Tracing
Manufacturer Abbott
Device ICD
Field Securesence
N° 3
Patient
This 37-year-old man received a Abbott Ellipse™ VR defibrillator for the management of hypertrophic cardiomyopathy complicated by episodes of sustained VT and episodes of AF with a rapid ventricular response. He was seen in consultation after receiving a shock in absence of loss of consciousness. Multiple episodes were recorded in the device memory.

Graph and trace
Tracing 3A
- irregular tachycardia with alternans between cycles classified VS, - , T1 and T2;
- the VT2 counter is filled; diagnosis of SVT (the 3 discrimination criteria are in favor of SVT: gradual onset, irregular ventricular rhythm, morphology similar to the reference QRS); inhibition of the therapies;
- VT2 counter filled in redetection (6 T2 classified cycles); diagnosis of SVT;
- interruption of EGM recording;
- new diagnosis of SVT;
- return to sinus rhythm was diagnosed and end of episode after 3 consecutive cycles classified VS;
Tracing 3B
- irregular tachycardia with alternans between cycles classified VS, - , T1 and T2;
- the VT1 counter is filled; diagnosis of SVT (discordance between parameters since sudden onset is present); inhibition of the therapies;
- return to sinus rhythm diagnosed and end of episode after 3 consecutive VS classified cycles;
Tracing 3C
- irregular tachycardia with alternans between cycles classified VS, - , T1 and T2;
- the VT2 counter is filled; diagnosis of SVT (the 3 criteria of discrimination are in favor of SVT: sudden onset, irregular ventricular rhythm, morphology similar to reference QRS); inhibition of the therapies;
- VT2 counter filled in redetection (6 T2 classified cycles); diagnosis of SVT;
- subtle acceleration of the tachycardia without change in morphology of the ventricular EGM; VF counter filled in redetection (6 F classified cycles); absence of discrimination; diagnosis of VF;
- ATP during the charge;
- at the end of the charge, absence of return to sinus rhythm; 30 J shock delivered on a short cycle (classified F);
- slowing of the rate and return to sinus rhythm;
Other articles that may be of interest to you


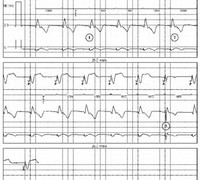


The morphology analysis has been completely modified in the recent devices manufactured by Abbott. In the older ICD, the morphology was based on an analysis of the bipolar detection channel (near-field), presenting several limitations, as the bipolar signal reflected only the local depolarization near the electrode. On the newer ICD, the bipolar channel is only used to synchronize with the reference pattern, since the morphology is analyzed on the discrimination channel (between the RV coil and the can or between the distal electrode and the can) enabling a finer discrimination. The far-field signal encompasses the overall depolarization of both ventricles and resembles the surface ECG. Based on comparisons with the reference pattern, a correlation score (percentage of similarity) is calculated for each QRS of the tachyarrhythmia, using eight regularly spaced points on the QRS complex (far-field channel). The update of the morphology is also more frequent and more progressive than on the older patterns.
These changes have significantly improved the performance of the algorithm. The latest guidelines recommend basing the single chamber discrimination on this morphology criterion only. These tracings illustrate the limits of the sudden onset criterion in the diagnosis of an episode of AF. The nominal programming (2/3) with the 3 criteria activated is the cause of several inappropriate therapies when AF becomes regular for a few cycles (sudden onset and regular rhythm in favor of VT). When the morphology criterion functions flawlessly, as in this patient, it may be advisable to limit the discrimination on this criterion only.
A second key point illustrated by these tracings is the rate limits within which discrimination must function. In ICD made by Abbott, since discrimination is not operative in the VF zone, the programming of the lower limit of that zone is critical. In this patient, the morphology analysis enabled an accurate diagnosis of SVT, regardless of the ventricular rate. A subtle rate acceleration and classification of the intervals in the VF zone triggered an inappropriate electric shock while the patient was conscious, which had a pronounced negative effect on his mood. To solve this problem, the professional practice guidelines recommend the programming of a VF zone from 250 bpm, with the ability to discriminate the origin of the arrhythmia up to a rate of ≥230 bpm.