Sensitivity and detection of arrhythmic events
In this article
The proper function of a defibrillator requires a flawless sensing of the rapid, low-amplitude signals of ventricular fibrillation (VF), without sensing a) cardiac signals other than the QRS and b) extra-cardiac signals. Consequently, the programming of sensitivity must be high and the refractory periods must be short. Unlike a pacemaker, the sensing threshold is not programmed at a fixed value; instead, it adapts automatically in reference to the amplitude of the preceding R wave. Sensitivity increases thereafter throughout the cycle, in search of a possible low-amplitude signal.
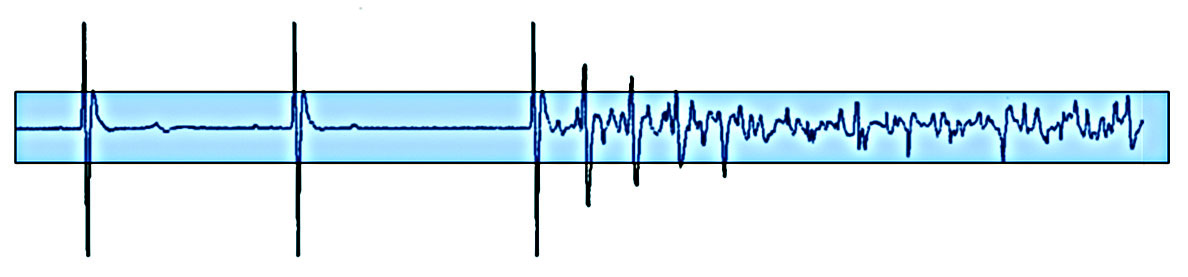

Once a signal has been sensed, at the end of the refractory period, the level of adaptation of the sensitivity starts at a programmable percentage of the sensed R wave amplitude, remains fixed during a programmable delay of adaptation, before increasing gradually to the programmed sensitivity level.
To provide accurate sensing of true VF without oversensing the T-wave during sinus rhythm, different settings for the following parameters can be modified:
- the sensed ventricular refractory period; this is not a real blanking period since the device is searching for the maximal amplitude of the signal after the sensing threshold has been reached; this refractory period has to be short (2 programmable values, 125 or 157 ms) to prevent the multiple sensing of a same depolarization signal, while preserving the ability to detect a very rapid tachycardia.
- the threshold start: upon expiration of the sensed refractory period, the sensing threshold automatically adjusts to a percentage of the maximum amplitude of the sensed signal with an absolute maximum value of 6 mV in the ventricle and minimal value of 1 mV. The post-sensed threshold start can be set at 50, 62.5, 75 or 100%. If the amplitude of the ventricular signal is > 6 mV, the threshold start is 6 mV if 100% or 3 mV if 50%. If the amplitude of the signal is < 1 mV, the threshold start is 1 mV.
- the decay delay: this parameter determines the amount of time after the sensed refractory period that the threshold remains at the programmed setting before beginning its decay to the programmed sensitivity level. The decay delay is programmable at 0, 30, 60, 95, 125, 190 or 220 ms.
- the maximum sensitivity
- low frequency attenuation : the advanced settings button enables to turn the Low frequency attenuation filter On or Off.

This figure shows the sensing circuit with a threshold start programmed at 50% and a decay delay at 0 ms.
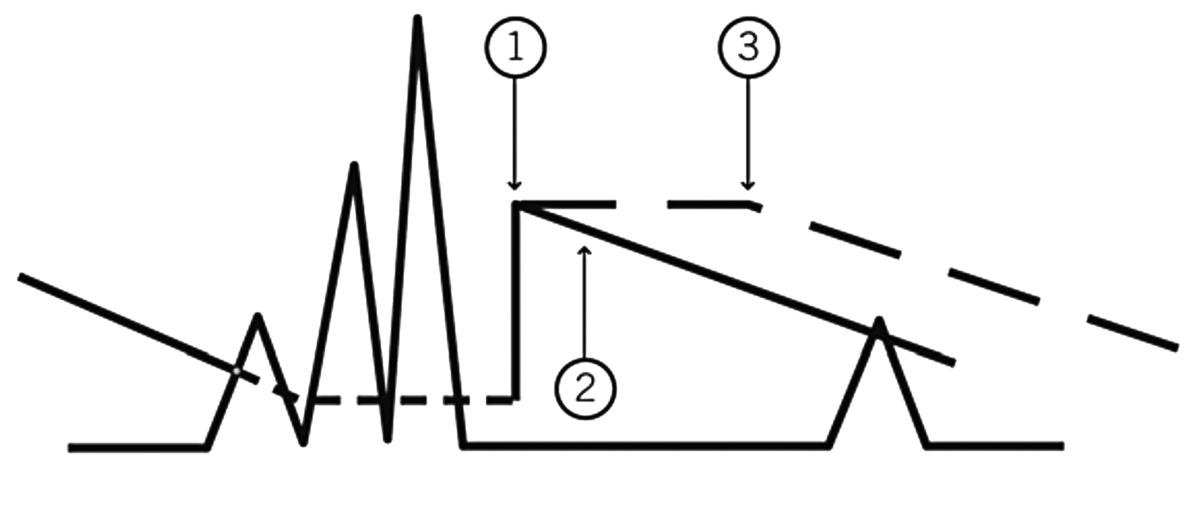
- Threshold Start
- Decay Delay of 0 ms
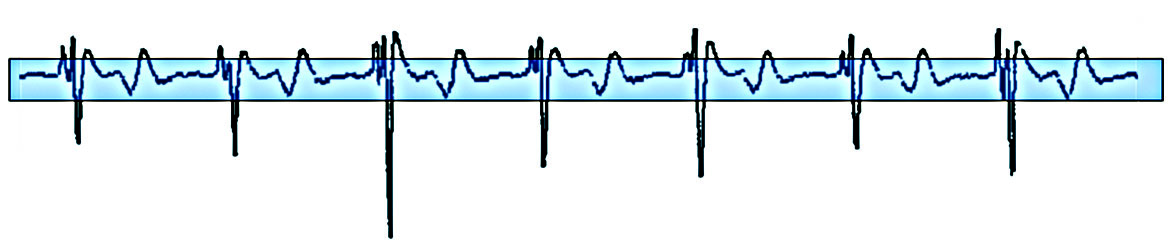
- Decay Delay of 60 ms
This figure shows the potential interest of prolonging the decay delay to avoid T-wave oversensing.
The nominal values of these different parameters depend on the programing of the low filters attenuation (LVA):
- LVA on: ventricular sensitivity 0.5 mV, threshold start 50%, decay delay 0 ms
- LVA off: ventricular sensitivity 0.3 mV, threshold start 62.5%, decay delay 60 ms
The choice of ranges of heart rates prompting interventions by a defibrillator is a critical programming step. State-of-the-art defibrillators enable the programming of several zones of arrhythmia detection based on the sensed RR intervals. Each zone has its own rate and duration criteria and can be specifically programmed with a view to identify and treat arrhythmias. The Detection Interval/Rate parameter is the interval/rate that must be exceeded within each rate zone to be counted toward detection of a tachyarrhythmia. Faster rates (in bpm) mean shorter cycle lengths (in milliseconds). The Detection Interval/Rate is independently programmable in each rate zone. Each detection interval must be at least 30 ms longer than the next fastest detection interval.
One to three detection zones can be configured at the discretion of the physician. Zones allow the clinician to deliver different therapies to rhythm disorders of different rates. In addition, a “Monitor Zone” can be set up where the ICD still evaluates the rhythm (diagnostics are collected and discriminators can be applied) but does not deliver therapy.
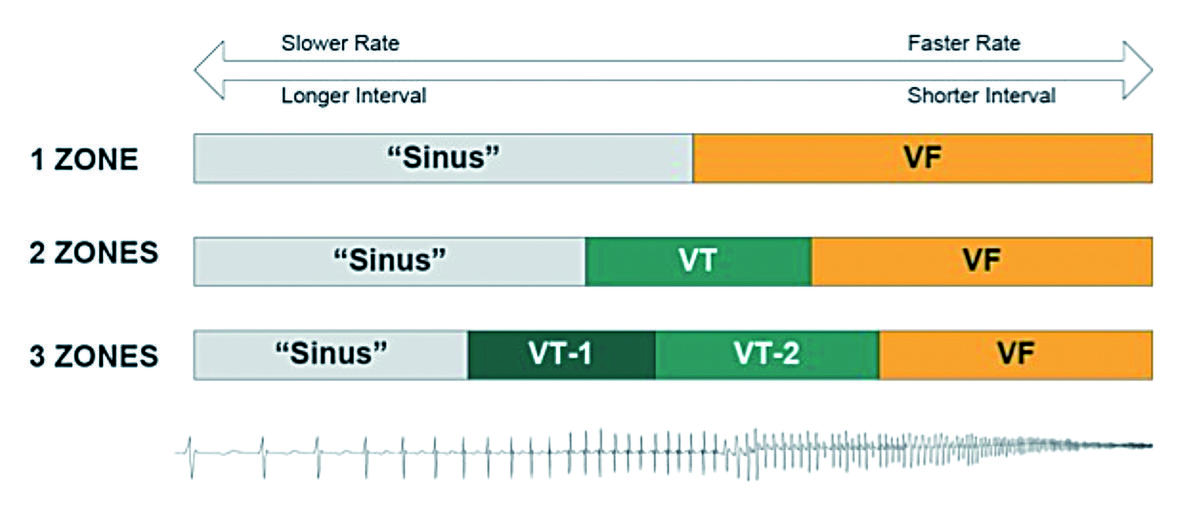
The number of zones and the range of rates programmed must be adapted to the patient’s characteristics, history and implant indications.
Secondary prevention:
In a patient presenting with heart failure, zones of heart rates are programmed as a function of the VT cycle prompting the device implantation. The programmed lower limit of the VT zone is usually 20 bpm below the rate of the clinical VT, as the introduction or addition of antiarrhythmic therapy after the defibrillator implantation might slow its rate.
Primary prevention:
In patients suffering from heart failure, the risk of developing VT after device implantation is high, probably justifying the programming of 2 zones of VT detection and treatment besides the VF zone. The choice of 2 distinct zones of VT has the distinct advantage of enabling the specific treatment of very rapid tachycardias, favoring painless anti-tachycardia pacing over the delivery of electric shocks. This was confirmed in the PAIN FREE I and II clinical studies, where anti-tachycardia pacing avoided 75% of shocks in the fast VT zone, significantly improving the quality of life without significantly increasing the rate of adverse events.
In patients presenting with complete atrio-ventricular block:
The risk of inappropriate therapy for supraventricular tachycardia is non-existent, allowing a relatively slow setting of the rates prompting interventions by the device, without lowering its specificity. Discrimination algorithms are, therefore, unnecessary, as all spontaneous tachycardias are ventricular in origin.
In young and active patients:
The risk of inappropriate therapy delivered for physiologic acceleration of the heart rate or for atrial fibrillation must be included in the decision to program several therapeutic zones, while attempting to limit the overlap of rates prompting defibrillator interventions and physiologic heart rates.
In patients presenting with Brugada syndrome:
The onset of organized VT is highly unlikely, whereas the risk of atrial fibrillation is increased. Consequently, the programming of a zone of detection and treatment of VT in addition to a VF zone is probably not only unnecessary, but also risky. The addition of a supplemental zone of monitoring allows the recording of slow tachy-arrhythmias, which helps adapting the programming. A single VF zone is usually programmed with a low inferior limit of this relatively high rate (>210 bpm) zone.
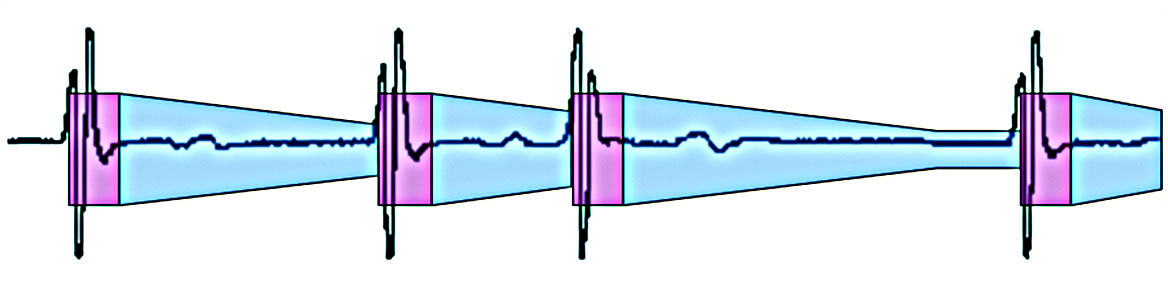
The classification of intervals is based on the instantaneous RR duration and the average of the last 4 cycles.
The ICD measures intervals and counts them in bins. An interval is the time period (in milliseconds) from one interval to the next (paced and/or sensed) in one chamber. The current interval (CI) is the interval of time between sensed ventricular events. The average interval (AI) is the average of the four most recent CIs.
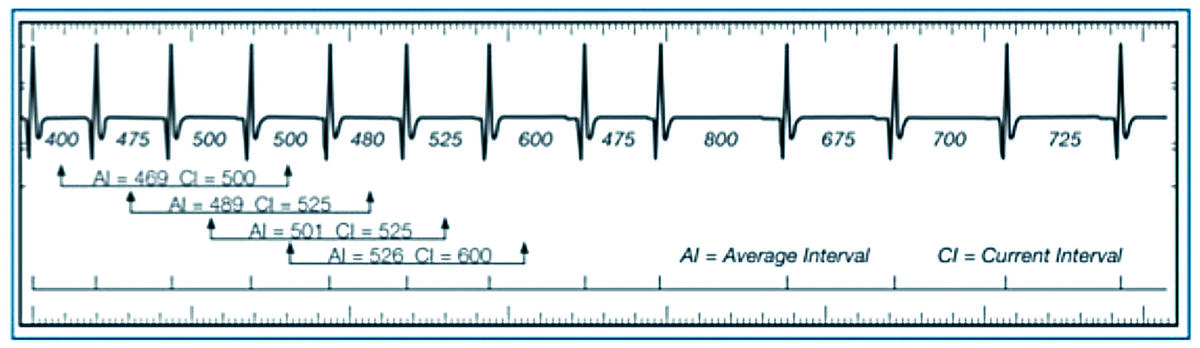
To bin an interval, the ICD needs to know how to classify it (VF, VT-1, VT-2, NSR [normal sinus rhythm]). If the average interval = the current interval, the interval is binned in that zone. If either the average interval or the current interval is classified as NSR, the interval is discarded. If the average interval and the current interval are different (but not NSR), the interval is binned in the higher zone.
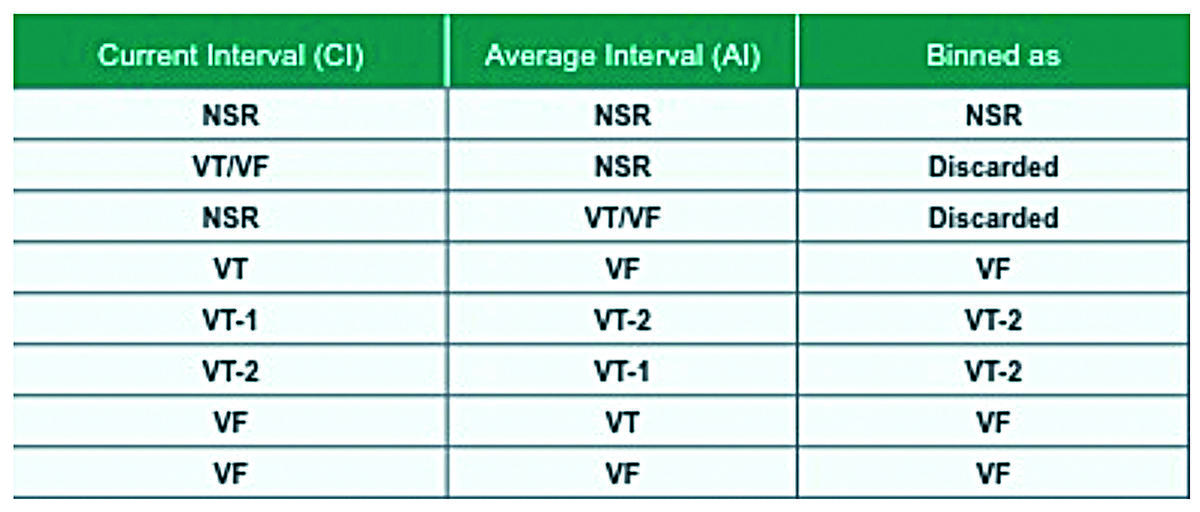
Intervals are counted until a bin reaches capacity. When a bin is full, that particular rhythm is “detected”.
All counters operate simultaneously:
- Slow VT counter (VT-1)
- Fast VT counter (VT-2)
- VF counter (VF)
- Return to sinus rhythm counter
An increment of the fastest zone counter does not increment the counter of the slower zones.
The first counter reaching the number of programmed cycles determines the detection, the type of event and, perhaps, the therapy(ies) delivered. These cycles are not necessarily consecutive. The same applies to post-therapy redetection, which has its own, separate counters.
For an episode to be terminated and another to be detected, the device must sense a return to sinus rhythm, defined by the number (3, 5 or 7; nominal = 5 cycles) of consecutive sinus cycles. If a cycle classified as VT or VF falls in-between VS, it resets the return to sinus rhythm counter to 0. With defibrillators older than Atlas II, a cycle in the monitor VT zone was classified as tachycardia and reset the return to sinus rhythm counter to 0. Since Atlas II, all cycles in the monitor VT zone a) are classified by this counter as cycles in the sinus zone, b) are counted by this counter, and c) do not reset the return to sinus rhythm counter to 0.
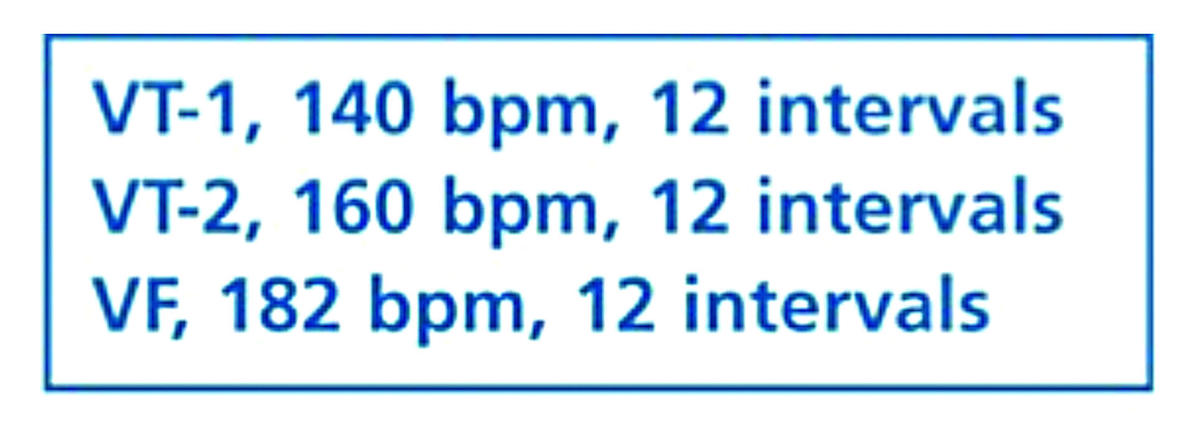
VT, VT-1, VT-2 or VF are programmable from 8 to 100 intervals in a bin.
1 Zone: nominal is defined as 12 intervals for the VF Zone
2 Zones: nominal is defined as 12 intervals for the VF Zone and 16 intervals for the VT Zone
3 Zones: nominal is defined as 12 intervals for the VF Zone, 16 intervals for the VT-2 Zone and 18 intervals for the VT-1 Zone
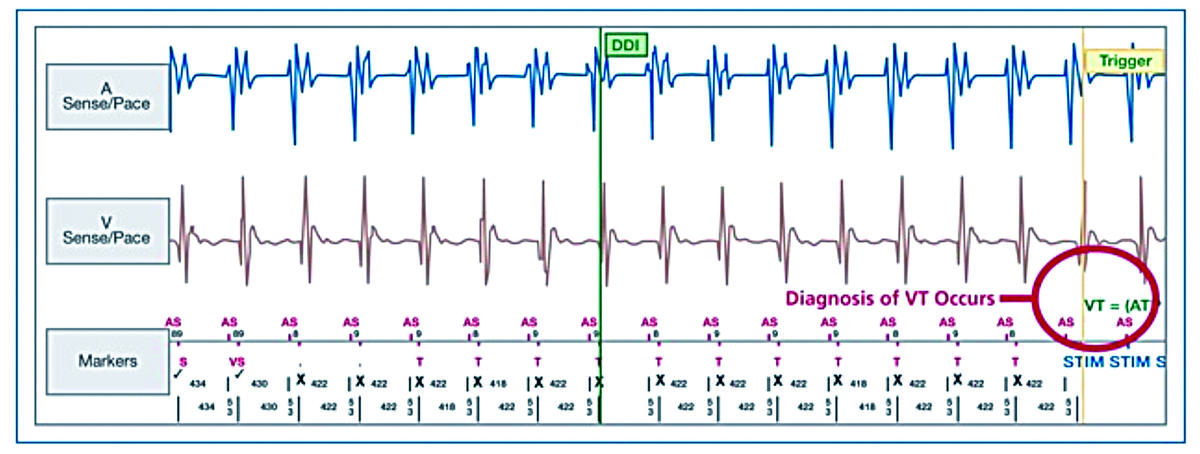
In this example, the device is set up in three zones, all bins set to 12 intervals. The 12th T is circled; that is the point where VT is diagnosed.
Sensing and detecting episodes Detection zones SENSING AND DETECTING EPISODES Auto-adjusting sensitivity The effective operation of an Implantable Cardioverter Defibrillator (ICD) relies on its ability to detect both fast ventricular signals and low amplitude ventricular fibrillation signals without detecting T waves or extra-cardiac signals when the patient is in sinus rhythm. In order to ensure appropriate sensing, the device should be programmed with a high sensitivity (low detection threshold) and short refractory periods. Unlike a pacemaker the detection threshold is not programmed to a fixed value. The detection threshold automatically adjusts based on the amplitude of the preceding R-wave. Following a sensed or paced ventricular event the detection circuit starts a blanking period...


