automatic mode switching
Tracing
Manufacturer Abbott
Device PM
Field Management of atrial arrhythmias
N° 32
Patient
64-year-old man, implanted with an AssurityTM + DR dual-chamber pacemaker for complete atrioventricular block; during the interrogation, highlighting of an AMS episode stored in the device memory.
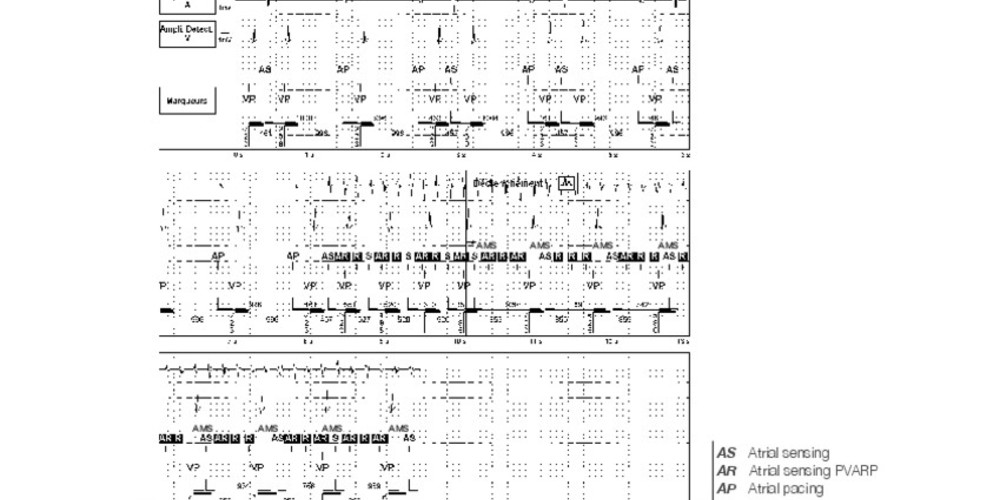
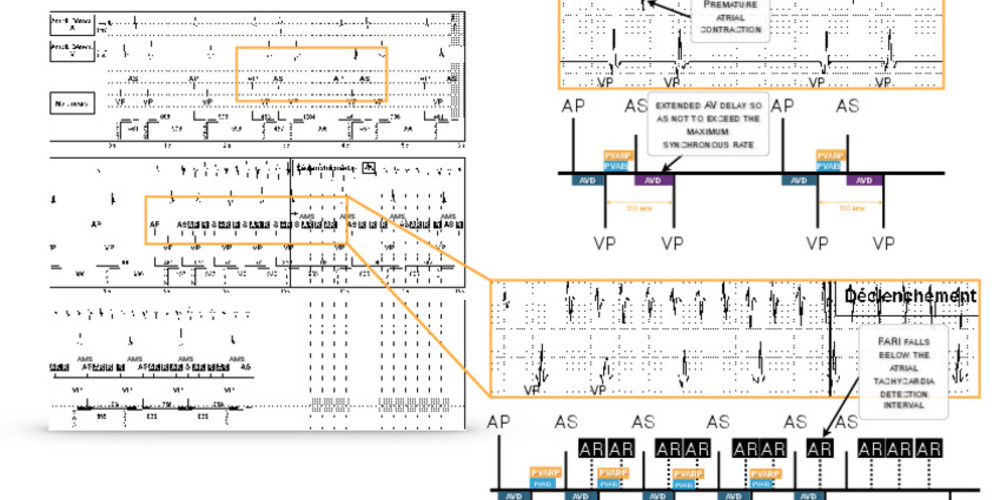
Graph and trace
Atrial pacing and ventricular pacing; classified (AS) premature atrial contraction followed by an extended AV delay so as not to exceed the maximum synchronous rate (130 beats/minute); onset of an atrial arrhythmia; each short atrial cycle decrements the filtered atrial rate by 39 ms; before mode switching, acceleration of the ventricular pacing rate; AMS when the filtered atrial rate interval (FARI) falls below the atrial tachycardia detection interval; slowing of the ventricular pacing rate.
Other articles that may be of interest to you



The management of pacemaker patients with atrial arrhythmia episodes is complex given the different types of mechanisms known to trigger atrial arrhythmias and the risk of runaway ventricular pacing due to sensing of a rapid atrial rhythm. The device can be programmed to respond to atrial arrhythmia by switching to an asynchronous mode in order to avoid high-rate ventricular pacing which can compromise hemodynamic stability. Mode switching is the ability of the pacemaker to automatically switch from an atrial tracking mode (DDD or VDD) to a non-atrial tracking mode (DDI or VDI). The ventricular pacing rate gradually progresses from the maximum synchronous rate to the response rate or the minimum rate. This avoids a sudden drop in the ventricular rate. Upon termination of the atrial tachyarrhythmia, mode switching reverts to the programmed synchronous pacing mode.
The ideal mode switching algorithm has the following characteristics: fast triggering to avoid prolonged rapid ventricular pacing during the initial detection phase of the arrhythmia; ability to quickly revert to a synchronous mode at the end of the arrhythmia episode; good atrial arrhythmia diagnostic capabilities even in the presence of atrial signals of varying amplitude and rate; ability to avoid mode switching in response to crosstalk, noise or sinus tachycardia.
The fallback algorithm used by AbbottTM pacemakers features certain specificities that are important to know. Automatic mode switching (AMS) uses a filtered, not actual, atrial rate based on a comparison of the current atrial rate with a continually updated average rate. Automatic mode switching (AMS) to DDI(R) or VVI(R) mode occurs when the filtered atrial rate surpasses the atrial tachycardia detection rate (ATDR). The pacemaker measures the actual PP interval at each cycle and calculates a filtered atrial rate interval (FARI) according to the following rule: if the actual PP interval is ≤ FARI, the FARI is decremented by 39 ms; if the actual PP interval is > FARI: the FAI is incremented by 23 ms. The atrial activities sensed in the PVARP, contrary to signals in the blanking period, are taken into account in the calculation of the FARI. Mode switching occurs as soon as the filtered atrial interval falls below the atrial tachycardia detection interval.
During mode switching, the pacing rate corresponds to the AMS base rate (programmable independently of the base rate) or the rate indicated by the sensor (rate response). The return to synchronous mode is only possible if the atrial rate falls below the maximum synchronous rate (FARI > the maximum synchronous rate interval) and not below the atrial tachycardia detection rate.
The criterion for recording AT/AF episodes is slightly different from that of AMS. The calculation method for the filtered atrial interval (FARI) is identical. To record an episode, 4 consecutive cycles with a PP interval and a FARI that are below the atrial tachycardia detection rate are needed. These consecutive cycles allow avoiding the recording of AMS episodes due to crosstalk (alternating short cycles-long cycles which can cause AMS but not the recording of the episode due to absence of consecutive short cycles). The AMS criterion is more sensitive than the recording criterion which is conversely more specific. Eight cycles with a PP interval and an FARI greater than the atrial tachycardia detection rate are thus needed for the episode to be terminated (2 episodes less than 20 seconds apart are considered as a single AT/AF episode).
The AT/AF burden is the percentage of time spent in AT/AF over a 52-week period. Each data point on the graph corresponds to the percentage of time the patient was in AT/AF over a seven-day period.