Loss of biventricular pacing due to VA crosstalk
Tracing
Manufacturer Medtronic
Device CRT
Field Standard parameters
N° 21
Patient
68-year-old man implanted with a triple-chamber defibrillator Viva XT CRT-D for dilated cardiomyopathy with atypical bundle branch block; routine follow-up; reduction of the percentage of biventricular pacing
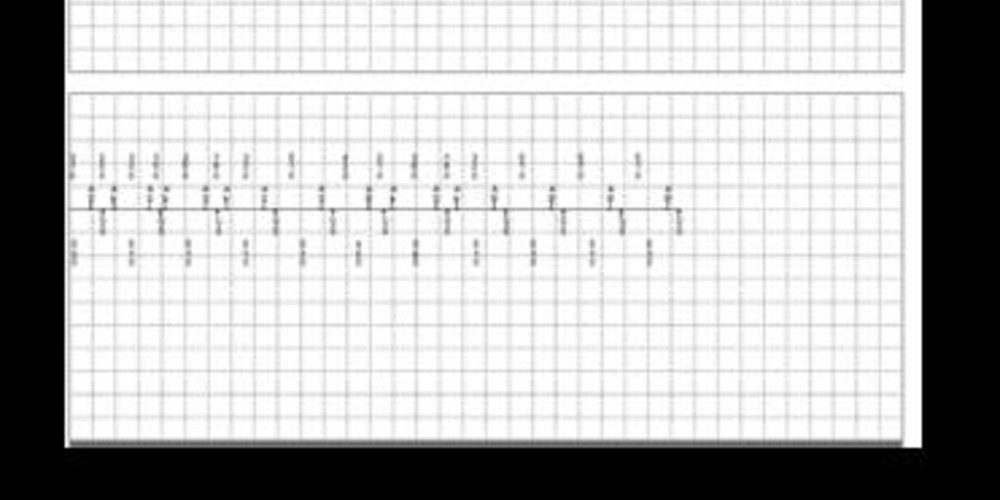
Graph and trace
Episodes of ventricular sensed event in the device memory
- 3 consecutive AR-VS cycles;
- commutation (MS: mode switch) to DDD mode with recovery of atrial synchronism;
- alternation of AS-BV-Ab cycles; probable VA crosstalk;
- commutation to DDIR (MS);
- asynchronous mode (DDIR) with no AV delay after an atrial sensed event; spontaneous ventricular events (VS);
Recording of an episode of AT/AF in the device memory - on the plot, typical railroad track pattern (alternation of 2 different atrial rates) compatible with VA crosstalk;
- far-field R-wave oversensing following the spontaneous ventricular depolarization; fixed AR-VS-Ab sequence, except for some cycles with a very short VS-Ab interval;
- intermittent interruption of the oversensing;
- commutation to a synchronous mode (MS);
- crosstalk restarts;
- diagnosis of AF and commutation to DDIR mode;
- absence of biventricular pacing (spontaneous ventricular events);
- diagnosis of AF made by the device for a duration of 20 seconds;
Tracing recorded during the consultation - biventricular pacing and crosstalk, the ventricular signal being sensed by the atrial channel in the PVARP (AR);
- decrease in atrial sensitivity (from 0.3 to 0.6 mV);
- crosstalk disappears.
Other articles that may be of interest to you

EGM recordings




In an implantable double or triple-chamber defibrillator, any pacing in one of the chambers (atrial channel or ventricular channel) generates a blanking in the other chamber (ventricular channel or atrial channel) to avoid the risk of crosstalk. The programming of long windows without sensing in the atrium following sensing or ventricular pacing increases the risk of undersensing of an atrial arrhythmia and limits the capabilities of the device to discriminate the origin of the atrial arrhythmias which is based on the comparison between atrial and ventricular rates. The optimization of post ventricular atrial blanking represents an essential step of the programming with the aim of finding a balance between proper sensing of atrial signals and minimal risk of crosstalk. In the new pacemaker and defibrillator platforms, 3 options are programmable:
The device memory and the electrograms of the recorded episodes must be systematically verified to confirm the diagnosis made by the device. In this patient, the defibrillator memory was saturated with short-duration episodes erroneously diagnosed as atrial arrhythmias in conjunction with crosstalk. These repeated episodes were responsible for a significant decrease in the percentage of biventricular pacing. A change in programming from partial to partial + did not correct the problem. On the other hand, a reprogramming of the constant atrial sensitivity to 0.6 mV was conversely effective.