Repetitive PMT due to crosstalk; diagnosis by remote monitoring
Tracing
Manufacturer Biotronik
Device PM
N° 13
Patient
78-year-old woman with an Evia DR-T dual-chamber pacemaker; telemedicine alert message (yellow) for high ventricular rate; summoning of the patient presenting signs of heart failure on arrival.
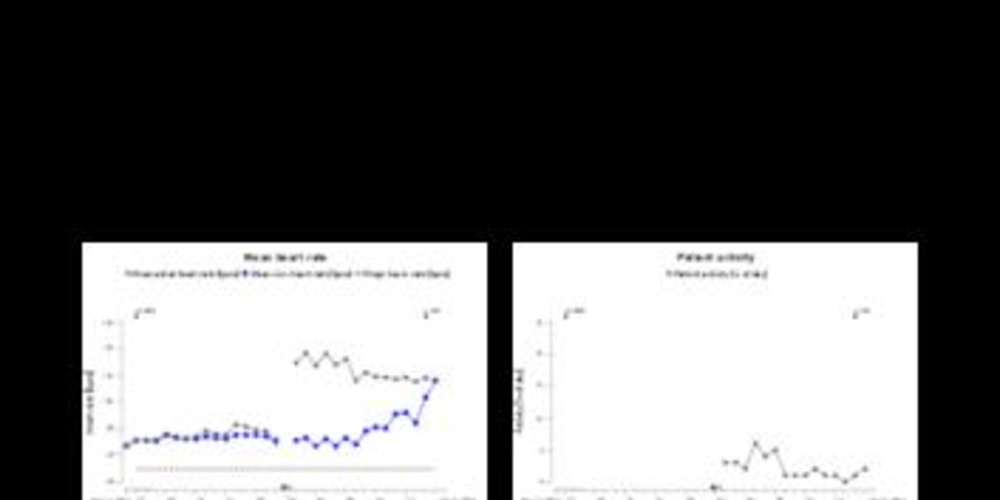
Graph and trace
Tracing 13a
- yellow alert for mean ventricular rate higher than the programmed limit (> 100 bpm);
- the telemedicine report shows a sudden increase in the percentage of ventricular pacing (from 0 to 100%) and a sudden increase in atrial and ventricular rate (rate equal to 116 bpm);
Tracing 3b
At arrival, recording of the tracing with 3 electrocardiographic leads, the atrial channel and the ventricular channel;
- atrial pacing and ventricular pacing with probable atrial and ventricular capture;
- probable crosstalk; the atrial EGM shows a signal sensed in the atrium outside of the refractory periods (AS) likely corresponding to ventricular depolarization subsequent to the pacing;
- the signal is classified as AS and is followed by an AV delay and ventricular pacing;
- new crosstalk although the signal is now sensed in the far-field period (no AV delay synchronized to this signal);
- probable retrograde conduction with atrial interval classified as AS generating an AV delay;
- probable PMT with succession of AS-VP cycles and constant VP-AS intervals; the atrial lead is positioned in the atrium (upper portion of the atrium), which explains the late sensing of atrial activity (depolarization from the lower portion of the atrium); the actual delay between the atrium and ventricular pacing is longer than that suggested by the short AV delay, thus explaining the possibility of a retrograde conduction (low atrial rhythm outside its refractory periods) and a PMT;
- after 8 consecutive cycles, suspicion of PMT; the device prolongs the AV delay by 50 ms;
- despite this change in AV delay, the VA interval remains constant: diagnosis of PMT;
- prolongation of the PVARP over one cycle; the retrograde conduction is sensed in the PVARP; no AV delay and termination of the tachycardia;
- identical perpetual reproduction of the same sequence.
Tracing 13c
- retrograde conduction test carried out in VDI mode at 90 bpm; presence of retrograde conduction with atrial activity sensed in the PVARP; relatively constant VA intervals.
Other articles that may be of interest to you





The initiation of a pacemaker-mediated tachycardia involves the programming of an atrial (DDD or VDD) monitoring mode, the permeability of retrograde conduction, a PVARP programmed shorter than the retrograde conduction and a momentary or permanent loss of atrioventricular synchrony. Indeed, if ventricular activity is correctly synchronized with that of the atrium, retrograde conduction is blocked. The maintenance of the PMT results from the sensing of a retrograde P' wave outside the refractory periods, which leads to the triggering of an often prolonged AV delay, which again fosters retrograde conduction after ventricular pacing. A PMT is therefore a repetitive sequence in which the pacemaker reacts to each retrograde P wave by pacing the ventricle at a high rate which in turn generates a retrograde P wave.
The cycle is thus repeated indefinitely unless there is appearance of a retrograde block or intervention of a specific algorithm. A PMT of prolonged duration may be poorly supported with symptoms ranging from a mild feeling of malaise or palpitations to cardiac decompensation in patients with an underlying heart disease. The rate of a PMT is contingent on the retrograde conduction time, the programmed maximum rate and the ongoing AV delay.
This tracing shows the specificities of the BiotronikTM devices in the management of PMTs:
This tracing also highlights the fact that if the triggering factor of the PMT is not corrected, the tachycardias can become incessant. In the present instance, remote monitoring has enabled a rapid diagnosis with a warning alert of increased mean ventricular rate. Upon arrival, the patient showed signs of heart failure, which were rapidly corrected after the change in programming and diuretic treatment. Atrial sensitivity was decreased (value was increased) in order to avoid crosstalk. Prolonging the PVARP beyond the retrograde conduction time (380 ms) was also possible in this patient with very limited exercise capacities (relatively low 2:1 point).