Repetitive pacemaker-mediated tachycardia
Tracing
Manufacturer Medtronic
Device PM
N° 19
Patient
83-year-old man implanted with an Adapta dual-chamber pacemaker for complete atrioventricular block; 4 days after discharge, consultation in the emergency room for palpitations; recording of this tracing; programming in DDDR mode.
Graph and trace
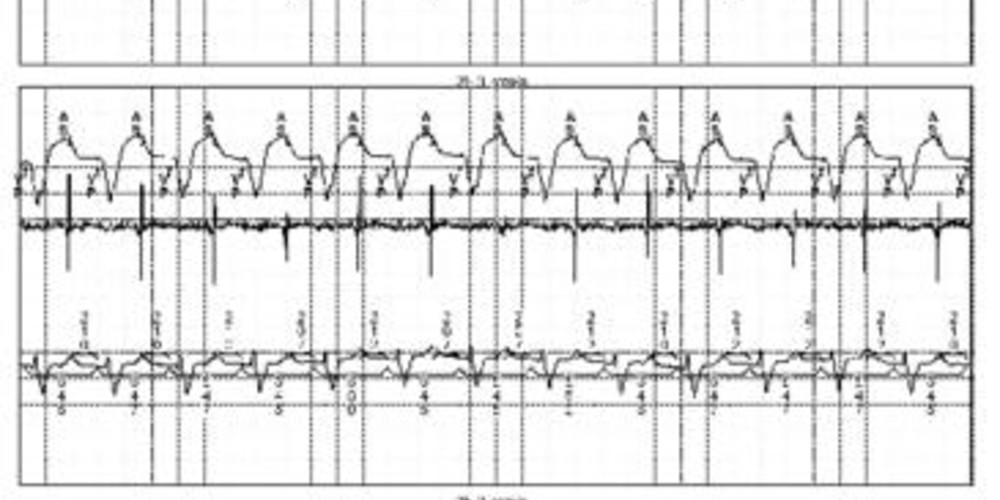
Tracing 19a: recording at patient arrival; the first line corresponds to lead I with the superimposed markers, the second line to the atrial EGM and the last line to lead II with the superimposed intervals;
- tachycardia at 110 beats per minute, the programmed maximal tracking rate; repetition of AS-VP intervals with prolongation of the AV delay (210 ms whereas the programmed AV delay on spontaneous atrial activity is 120 ms) so as not to exceed the programmed maximum rate; this may represent either a sinus tachycardia (unlikely, patient at rest and no reason for the AV delay to be prolonged), a relatively slow atrial tachycardia or pacemaker-mediated tachycardia;
Tracing 19b: the initial interrogation showed that the intervention algorithm due to PMT was not programmed (OFF, nominal programming); programming of this algorithm and recording of the EGM;
- same tracing as above;
- programming of the algorithm;
- diagnosis of PMT determined by the device: 8 consecutive intervals where the VA interval is less than 400 ms (340 ms in this patient), the VA interval begins with a paced ventricular event, the VA interval ends with a sensed atrial event and slow capture rate; anti-PMT intervention: prolongation of the post-ventricular atrial refractory period to 400 ms; the atrial activity is sensed in this refractory period and is not synchronized to ventricular activity by the pacemaker;
- atrial and ventricular pacing (AP-VP) with short AV delay; this short AV delay is secondary to a non-competitive atrial pacing (NCAP) automatically activated during one cycle after the ninth ventricular pacing of a PMT episode; this function shortens the next paced AV delay to maintain a stable ventricular rate;
- termination of the tachycardia and paced atrioventricular rhythm (AP-VP).
Other articles that may be of interest to you
EGM recordings




The initiation of a pacemaker-mediated tachycardia (PMT) involves the programming of an atrial tracking mode (DDD or VDD), the permeability of the retrograde conduction and a momentary or permanent loss of atrioventricular synchrony. Indeed, while ventricular activity is properly synchronized with that of the atrium, retrograde conduction is blocked. Maintenance of the PMT results from the sensing of a retrograde P wave outside the refractory periods, which leads to the triggering of an often prolonged AV delay, which again favors retrograde conduction after ventricular pacing. A PMT is thus a repetitive sequence in which the pacemaker reacts to each retrograde P wave by pacing the ventricle at a high rate which in turn generates a retrograde P wave.
The cycle hence repeats itself indefinitely unless there is a retrograde block or the intervention of a specific algorithm. A prolonged PMT may be poorly supported with symptoms ranging from simple feeling of uneasiness or palpitations up to cardiac decompensation in patients with underlying cardiac disease. The rate of a PMT is contingent on the retrograde conduction time, the maximum programmed rate and the current AV delay.
This tracing corresponds to a PMT episode and allows emphasizing certain elements of the functioning of dual-chamber MedtronicTM pacemakers: