Reveal Linq in a patient with syncope
Tracing
Manufacturer Medtronic
Device ILR
Field Reveal Linq
N° 15
Patient
50-year-old woman with sudden syncopal episodes complicated by trauma with complete negative etiological assessment (electrocardiogram, echocardiography, Holter-ECG, tilt-test, electrophysiological study); implantation of a Reveal LINQ and discharged home; a few months after discharge, remote transmission report of detected episodes with diagnosed Symptom, Pause and Brady.

Graph and trace
This report transmitted remotely provides a certain amount of information:
- the degree of wear of the batteries; in this patient, implantation is recent and there is no wear (Battery: OK);
- a few seconds of ECG highlight a sinus rhythm with narrow QRS;
- the event counter shows that this patient presented multiple events labeled Pause Brady and, since the previous interrogation, a pause episode and a symptomatic episode;
- a 90-day Cardiac Compass report; this report is similar to that obtained during interrogation of a pacemaker or MedtronicTM defibrillator with analysis of AF load, heart rate, heart rate variability and activity; (rate, frequency) histograms are also found; this graph does not find any particular abnormalities for this patient;
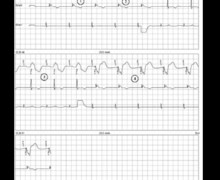
This patient presented a recurrence of syncope which triggered the recording. At the same time, the device diagnosed a pause. As in a defibrillator tracing, the episode generates a graph and EGM;
- the tracing shows a complete AV block episode with multiple blocked P waves and a prolonged pause.
Other articles that may be of interest to you


In this patient, the demonstration of a prolonged pause due to complete AV block led to the implantation of a cardiac pacemaker after an exhaustive etiological assessment, which suppressed the recurrences of syncope.
The commercial introduction of Reveal LINQ is part of the development of nanotechnologies with miniaturization of the device and the possibility of remote interrogation. The basics of operation do not significantly differ from previous platforms with automatic or patient-activated recordings. There are, however, a number of noteworthy developments. The reduction in size facilitates implantation possibilities in young children and represents a considerable cosmetic advantage with very limited scar size (<1 cm) and less noticeable lump.
The principal modification resides in the implantation technique. The device is delivered with a specific implant kit (the insertion tool is preloaded with the device) allowing a simplified mini-invasive procedure of limited duration. In short, the reduction in the size of the device allows envisioning implantation outside of traditional structures (operating room, implantation room for pacemakers). There are two optimal sites for implantation of the device allowing insertion without preoperative body surface mapping. Indeed, experience shows that these 2 positions allow sufficient tracing quality for a majority of patients.
As first choice, the recommended site is located at the fourth intercostal space, about 2 cm from the left side of the sternum at a 45° angle. If this site does not provide an acceptable tracing quality, a second site (at the fourth intercostal space, approx. 2 cm from the left side of the sternum but without an angle and therefore parallel to the septum) can be tested. The incision may be made at either end of these recommended insertion sites depending on physician preference, patient anatomy, comfort and cosmetic considerations. If for any reason (localized dermatological problem, for example) it is necessary to implant the device in a different site, it is then recommended to perform surface mapping prior to insertion in order to verify that the quality of the signal and the detection of R wave amplitude are acceptable. When an insertion site in the inframammary fold (angle 90 degrees to the sternum in the fifth intercostal space region) is proposed for cosmetic reasons, it is then necessary to validate the quality of the signals collected in pre-implantation. For this purpose, 2 ECG electrodes are positioned at 4 cm distance in order to match the electrode spacing of the device.
Once the device is positioned, it is necessary to verify the quality of the recordings. The aim is to obtain stable amplitude R waves with a minimum amplitude of 0.3 mV and a peak-to-peak R wave amplitude at least greater than twice the peak-to-peak amplitude of both T and P waves.
Once implanted, the patient is given the Model 9538 Patient Assistant (Portable Activator) for recording of symptomatic episodes, as well as the device reference and identification card and the MyCareLink Patient Monitor, which allows remote monitoring via a cell telephone link.