Unsuccessful antitachycardia pacing followed by electrical shock for VT
Tracing
Manufacturer Boston Scientific
Device ICD
Field Therapy
N° 8
Patient
This 84-year-old man presenting with ischemic cardiomyopathy underwent implantation of a Boston Science Teligen dual chamber defibrillator for secondary prevention of VT. He suffered from chronic AFib and abnormal atrioventricular conduction. He was seen for a complaint of palpitation followed by near syncope and delivery of an electrical shock.
Summary
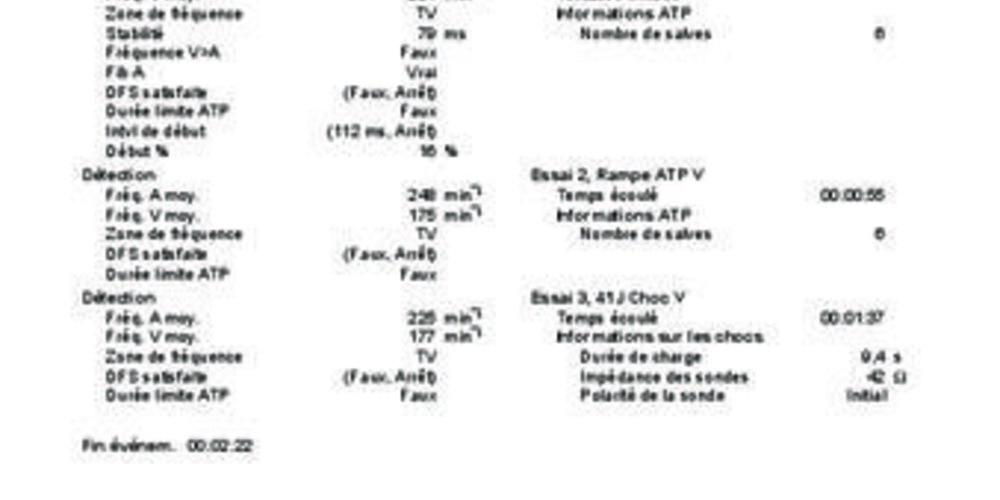
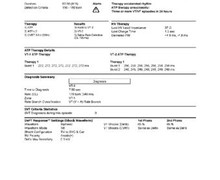
Episode of VT that prompted 2 consecutive series of 6 bursts of unsuccessful ATP followed by a 41-J electrical shock.
Graph and trace
Tracing
- AFib with rate responsive ventricular pacing in mode switch;
- ventricular pair;
- sudden acceleration of the ventricular rate;
- 8 out of 10 criterion fulfilled;
- end of Duration. The first therapy programmed for the VT zone was not delivered because of instability of the ventricular rhythm, as the atrial rhythm was AFib. The device diagnosed conducted AFib and withheld the therapy. However, with AV conduction being markedly abnormal, the diagnosis of dual tachycardia (Afib + VT) was very likely;
- stabilization of the ventricular rhythm and diagnosis of VT;
- first burst of 8 cycles of ATP; an analysis of the EGM suggested failure of ventricular capture during the burst; indeed, the device was pacing though did not capture the ventricle and the spontaneous ventricular events are visible;
- unsuccessful burst;
- second burst of 10 cycles of ATP; capture continued to be doubtful;
- unsuccessful burst;
- third burst of 12 cycles of ATP; capture continued to be doubtful;
- unsuccessful burst;
- fourth burst of 14 cycles of ATP; capture continued to be doubtful;
- unsuccessful burst;
- fifth burst of 14 cycles of ATP; capture still doubtful;
- unsuccessful burst;
- sixth burst of 14 cycles of ATP; capture still doubtful;
- unsuccessful burst;
- first ramp of 8 cycles of ATP with 5-ms decrement between the stimuli. Capture still doubtful;
- unsuccessful ramp;
- second ramp of 10 cycles of ATP; 5-ms decrement between the stimuli; capture still doubtful;
- unsuccessful ramp;
- third ramp of 12 cycles of ATP; 5-ms decrement between the stimuli. However, the programmable pacing interval was limited to 220 ms. When this limit was reached, the pacing cycle remained at 220 ms; capture still doubtful;
- unsuccessful ramp;
- fourth ramp of 14 cycles of ATP; shortest cycle limited to 220 ms; capture still doubtful;
- unsuccessful ramp;
- fifth ramp of 14 cycles of ATP; shortest cycle limited to 220 ms; capture still doubtful;
- unsuccessful ramp;
- sixth ramp of 14 cycles of ATP; shortest cycle limited to 220 ms; capture still doubtful;
- unsuccessful ramp;
- persistence of tachyarrhythmia and onset of the charge of the capacitors;
- end of the charge;
- delivery of 41-J electrical shock;
- successful shock. VT and AFib were both terminated.
Other articles that may be of interest to you
EGM recordings
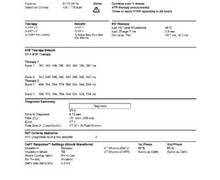


The various sequences of ATP did not end this arrhythmic episode. Analysis of the EGM revealed a failure to capture during the sequences, explained either by an elevation of the pacing threshold or by an inability to capture a sufficient amount of myocardium during the tachycardia. During sinus rhythm, the pacing threshold was 1.0 V/0.4 ms, considerably below the output delivered during a sequence of ATP. Consequently, this was probably not due to an insufficient quantity of energy delivered, rather than an inability to capture the ventricles by pacing during the tachycardia. A different pacing rate and an increase in the number of stimuli might have restored a reliable capture though this is not certain.
In the VT zone, the therapies succeed each other in case of successive failures. The series ends as soon as the rhythm is considered slow again, or when all therapies have been exhausted. The choice of strength of the first shock after sequences of ATP is debatable. It can be empirically programmed at a low amplitude and terminate the tachycardia while limiting the discomfort caused by the electrical shock and limiting the consumption of energy. The shock must not be too weak (<5V), and be below the upper limit of vulnerability neither in the atrium nor in the ventricle, because of the risk of inducing AFib or VF. An alternative consists of programming, as in this patient, a first shock of maximum strength in order to increase the likelihood of VT termination at first attempt, to minimize the number of shocks delivered, and to increase the likelihood of converting AFib, should the shock be inappropriate.