AdaptivCRT programming in a patient with a normal PR interval
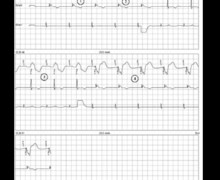
Tracing
Manufacturer Medtronic
Device CRT
Field AV & VV delays optimization
N° 11
Patient
65-year-old man implanted with a triple-chamber defibrillator Viva XT CRT-D for idiopathic dilated cardiomyopathy with left bundle branch block; 3 months post implant interrogation.

Graph and trace
The first line corresponds to an electrocardiographic lead with superimposed markers, the second line to the bipolar right ventricular EGM (EGM3) and the third line to the bipolar atrial recording (EGM1);
- atrial and biventricular pacing (AP-BV) without AdaptivCRT function;
- programming of the AdaptivCRT algorithm to Auto Bi-V and LV mode;
- temporary prolongation of the AV delay to 300 ms; 5 consecutive AP-VS cycles with a LBBB morphology; the delay between the atrial pacing and the bipolar right ventricular EGM is less than 250 ms;
- LV pacing with fusion.
Other articles that may be of interest to you