Basic concepts
LEFT VENTRICULAR STIMULATION
The left ventricle can be stimulated from 4 different approaches: 1) subepicardial, with the lead implanted transvenously via a coronary sinus tributary, 2) endocardial, with the lead implanted transseptally, 3) epicardial, with the lead implanted surgically, and 4) intrapericardial, with the lead implanted transcutaneously. The transvenous approach is used preferentially in the majority of medical centers. The coronary sinus drains nearly the entire left ventricle from 4 main tributaries: 1) the inferior, the posterior, the lateral, and the great cardiac vein(s). The anterior aspect of the left ventricle and the septum are drained by the anterior interventricular vein, while the lateral walls are drained by the postero-lateral, antero-lateral and lateral veins. The atria are also drained by several veins (of which the main is the vein of Marshall) into the coronary sinus. The length, diameter and orientation of the coronary sinus are highly variable; consequently, the challenge represented by each device implantation is unpredictable. Several valves may obstruct or narrow the coronary sinus. The valve of Thebesius is near the ostium, while that of Vieussens is near the ostium of the first postero-lateral vein. The phrenic nerve courses along the lateral veins, along the posterior branches of an anterolateral vein, and along the anterior branches of a postero-lateral vein.
The several steps of a device implantation procedure include the a) venous access, b) introduction of a guiding sheath in the right atrium, c) cannulation of the coronary sinus, d) opacification and selection of the target vein, e) implantation of the lead, and b) removal of the sheath. In recent years, new leads of various shapes and sizes have been developed. Once the venous network has been opacified, a stimulation lead is chosen that corresponds closely to the anatomical characteristics of the target vein. This choice is determined by the sizes of the ostium and body of the target vein, such that the lead diameter and size of the vascular internal lumen fit tightly. Some variables, such as a high capture threshold or the likelihood of diaphragmatic stimulation are unpredictable, though, ultimately, have an influence on the choice of stimulation site and, therefore, on the choice of optimal lead.
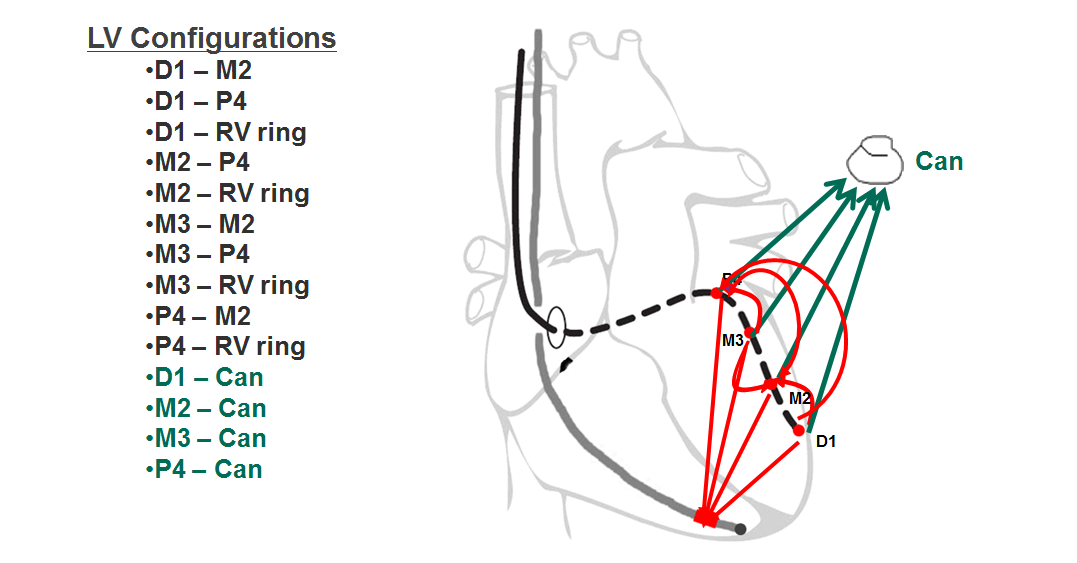
Configuration of left ventricular stimulation
The various programming options available enable the selection of a LV stimulation polarity associated with a reliable and durable myocardial capture with the least amount of power necessary in order to maximize the longevity of the device, without stimulating the phrenic nerve. The programming of the stimulation amplitude must optimize the battery life while preserving a sufficient safety margin. The LV epicardial stimulation threshold is often higher (twice as high in one study) and more variable than the RV stimulation threshold. It might not be possible to obtain a safety margin as high as twice the capture threshold since, when >2.0 V, the batteries will likely be prematurely depleted. In some patients the stimulation amplitude and pulse width must be meticulously programmed to capture the left ventricle without phrenic nerve stimulation. The influence of the LV stimulation configuration on the quality of response to cardiac resynchronization remains to be determined and rarely represents a selection criterion.
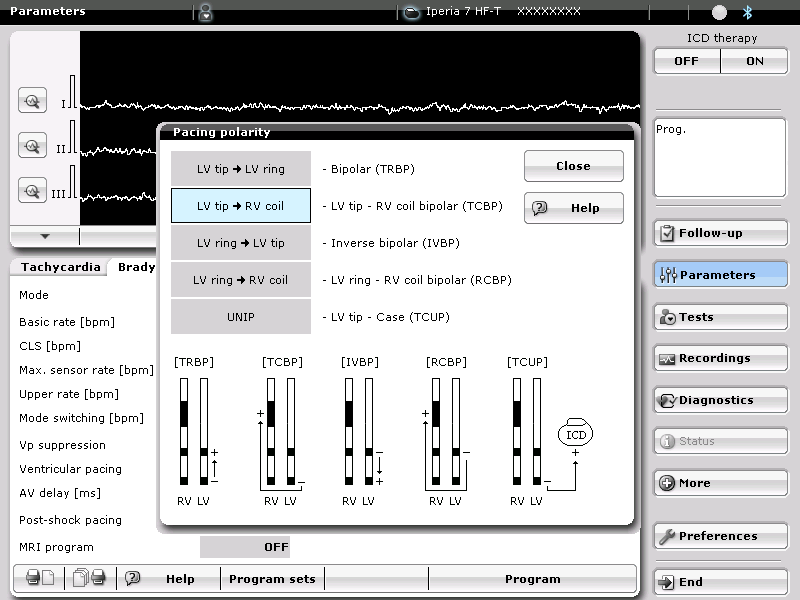
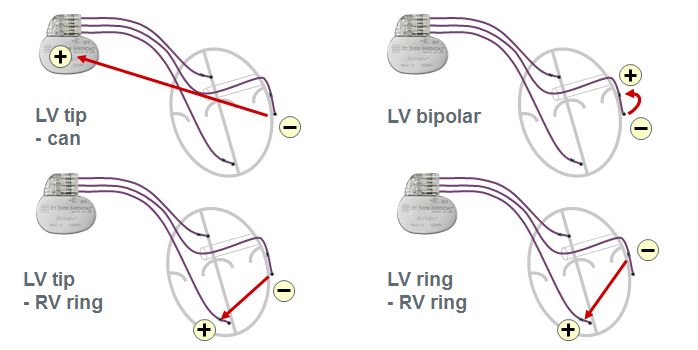
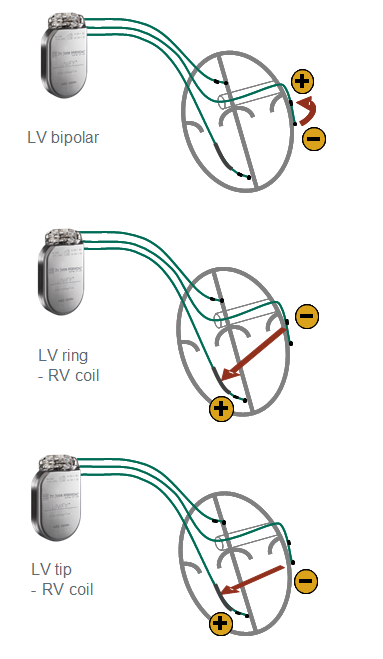
The armamentarium offered by the various device manufacturers includes uni-, bi- and quadripolar LV leads. The stimulation polarity is programmable in the left ventricle by choosing a quadripolar (4 electrodes) or non-quadripolar (1 or 2 electrodes) lead. If a unipolar LV lead is implanted, a single configuration (LV tip à RV ring or RV coil) might be programmable depending on the manufacturer and type of device. With most defibrillators, the RV coil is used instead of the RV ring. With CRT-P, the RV ring (proximal electrode of a bipolar lead) is used. With some devices and, depending on the manufacturer, the pulse generator may participate in the stimulation vector, offering the programming of LV tip à pulse generator (can) as second choice of stimulation configuration. If a bipolar LV lead is implanted, between 3 and 6 configurations are available depending on the manufacturer and type of device. The threshold is often higher with LV ring à RV coil configuration and the distal LV electrode (cathode) is preferentially used as the active electrode, while the RV coil or LV ring (anode) are used as the indifferent electrode. If a quadripolar LV lead is implanted, between 12 and 17 configurations are available depending on the manufacturer and the type of device. This multitude of choices allows an optimization of the capture threshold and a lower likelihood of phrenic nerve stimulation. With a wide spacing of the electrodes, the activation sequence can be varied, for example by choosing a distal (apical) versus proximal (basal) electrode. This choice may have a positive impact on the response rate, despite the paucity of criteria objectively predictive of the quality of response to therapy. St. Jude Medical makes the only devices, which offer a choice of dual site LV stimulation, as an increase in the number of stimulated sites is likely to decrease the activation dyssynchrony.
Anodal capture
The pulse strength influences the likelihood of anodal capture. The cathode at the tip of the LV lead is usually smaller than the anode, explaining the high current density at that site. A strong pulse may create a high enough current density to capture the tissue near the anode. The RV ring of CRT-P is often used as anode to stimulate the left ventricle. A high-amplitude stimulation may cause an anodal RV capture resulting in triple-point stimulation: LV and RV cathodes + RV anode. Anodal capture is more likely when the LV stimulation configuration includes a true RV bipolar lead (lead ring) instead of an integrated bipolar lead (since the anode is the distal coil), probably because the small size of the ring promotes a higher current density. The electrocardiographic morphology is often slightly modified compared with the usual BiV appearance. A 12-lead electrocardiogram, instead of the single channel of the programmer, is usually needed for the diagnosis. On the other hand, an anodal capture may considerably modify the analysis of the tracings during the LV threshold test. The hemodynamic effect of this type of stimulation, which increases the number of stimulated sites, might be positive, though the clinical results remain to be seen. An anodal capture usually requires strong stimulation pulses, which shorten the devices’ life expectancy.
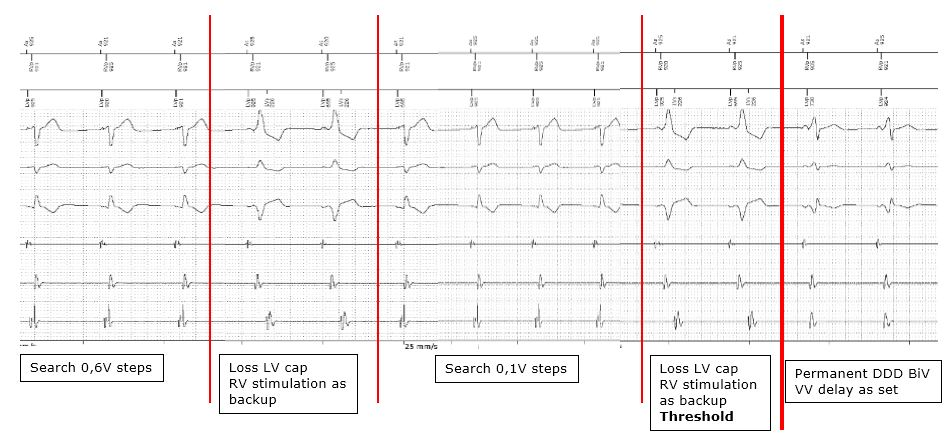
Automated left ventricular threshold
The function of the automated LV threshold is often very close to that described for the RV lead. The threshold measurement is based on the analysis of the evoked response, or by observing the synchronization of the RV events sensed after a stimulated LV event. The threshold is measured at regular intervals of between 8 and 24 h, depending on the manufacturer, after which a safety margin is programmed, without further cycle-by-cycle verification of capture. It is noteworthy that triple chamber devices do not verify the cycle-by-cycle LV or RV lead capture.